Postsurgical hemorrhage refers to excessive bleeding after a surgical procedure, which can occur due to various causes. It is a major complication that requires prompt identification and management to prevent life-threatening consequences. Whether occurring immediately after surgery or in the days that follow, controlling postsurgical hemorrhage is essential for optimizing patient recovery and reducing morbidity and mortality.
Types of Postsurgical Hemorrhage
1. Primary Hemorrhage
Primary hemorrhage occurs within the first few hours after surgery. It is often related to surgical factors such as inadequate hemostasis, injury to blood vessels, or clotting abnormalities. The bleeding typically involves large vessels that were not adequately ligated or controlled during the operation.
2. Secondary Hemorrhage
Secondary hemorrhage is typically seen 24 hours to several days post-surgery. It can result from delayed bleeding due to infection, dislodgement of clots, or slippage of ligatures. This type of hemorrhage may be more challenging to identify, as the initial hemostatic measures may seem sufficient at first.
Causes of Postsurgical Hemorrhage
1. Inadequate Hemostasis
Inadequate hemostasis during surgery is the leading cause of postsurgical hemorrhage. Surgical procedures, particularly those involving major blood vessels or tissues rich in blood supply, can result in bleeding if blood vessels are not properly ligated or sealed.
2. Coagulopathy
Patients with underlying bleeding disorders, whether congenital (like hemophilia) or acquired (such as liver disease or anticoagulant use), are at increased risk of postoperative bleeding. Coagulopathy can also develop as a result of massive transfusions or certain medications administered during the perioperative period.
3. Infection and Inflammation
Infection can exacerbate bleeding, particularly if the surgical site becomes infected, leading to delayed hemorrhage. Inflammatory processes may erode blood vessels or dislodge clots, resulting in secondary bleeding.
4. Vessel Injury
Direct injury to blood vessels during surgery can cause immediate or delayed bleeding. Whether accidental or intentional, vascular injuries must be promptly managed to prevent significant blood loss.
Risk Factors for Postsurgical Hemorrhage
Certain factors increase the likelihood of postsurgical hemorrhage. These risk factors must be assessed preoperatively to optimize management strategies.
- Use of Anticoagulants or Antiplatelet Drugs: These medications prevent blood clotting and can significantly increase the risk of excessive bleeding.
- Pre-existing Bleeding Disorders: Conditions like hemophilia, von Willebrand disease, or platelet dysfunction contribute to poor clotting ability.
- Surgical Site and Type of Procedure: High-risk procedures, such as cardiovascular, liver, or orthopedic surgeries, are more likely to result in significant blood loss.
- Age and General Health Status: Older patients or those with chronic health issues, such as diabetes or hypertension, have a higher risk of hemorrhage and complications during recovery.
- Obesity: Increases the technical difficulty of surgery and may compromise blood vessel access, leading to a higher risk of bleeding.
Symptoms and Signs of Postsurgical Hemorrhage
Recognizing the signs of postsurgical hemorrhage is crucial for effective intervention. Symptoms can vary depending on the severity of the bleeding, but common indicators include:
- Excessive Blood Loss: A sudden or progressive increase in blood loss, particularly if it surpasses normal postoperative expectations.
- Tachycardia and Hypotension: Low blood pressure and increased heart rate are early signs of hypovolemia, which may indicate significant blood loss.
- Pallor and Weakness: As blood volume decreases, patients may exhibit signs of shock, including dizziness, weakness, and extreme pallor.
- Pain at Surgical Site: An increase in pain, particularly if associated with swelling or changes in the appearance of the wound, may suggest hemorrhage.
Diagnostic Measures for Postsurgical Hemorrhage
To identify the source and extent of postsurgical hemorrhage, several diagnostic techniques are employed:
1. Physical Examination
A thorough examination of the surgical site is critical. Clinicians will assess for visible blood accumulation, swelling, or hematoma formation. Signs of infection, such as redness and warmth, may also indicate an underlying complication contributing to the bleeding.
2. Blood Tests
Routine blood tests, including a complete blood count (CBC), coagulation profile, and crossmatching, are essential to evaluate the severity of blood loss, detect coagulopathies, and determine the need for transfusion.
3. Imaging
If the source of bleeding is not obvious, imaging studies like ultrasound, CT scans, or MRI may be used to identify hematomas, vascular injury, or retained blood within the surgical area.
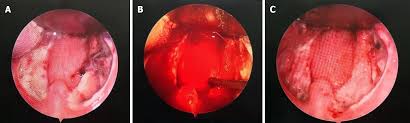
4. Endoscopy or Angiography
In cases of suspected internal bleeding or vascular injury, endoscopic examination or angiography may be performed to locate the source of hemorrhage.
Management of Postsurgical Hemorrhage
The management of postsurgical hemorrhage is a multi-step process that may involve conservative measures, surgical intervention, and blood product administration.
Step 1: Initial Stabilization
- Airway and Breathing: Ensure that the patient’s airway is secure and that they are receiving adequate oxygenation.
- IV Fluids: Administer crystalloids (e.g., saline or Ringer’s lactate) to replace lost volume and improve circulation.
- Blood Transfusion: If the patient’s hemoglobin levels drop significantly or if there is evidence of shock, transfusions of packed red blood cells (PRBCs) may be necessary.
Step 2: Identifying and Controlling the Bleeding Source
- Conservative Management: In some cases, compression or packing can temporarily control bleeding until further intervention is possible.
- Surgical Intervention: If conservative measures fail, surgical exploration may be required to locate and repair the source of bleeding, including the ligation of vessels or removal of hematomas.
- Endovascular Interventions: Angiographic embolization can be performed to control bleeding in cases of vascular injury without the need for open surgery.
Step 3: Preventing Future Episodes
Patients who have experienced postsurgical hemorrhage are at increased risk of recurrence. Monitoring and addressing any underlying issues, such as coagulopathies, infection, or vessel damage, is vital for preventing further episodes.
Prevention of Postsurgical Hemorrhage
Preventing postsurgical hemorrhage involves careful planning and proactive management strategies.
- Preoperative Evaluation: Identifying patients at high risk of bleeding through history, physical examination, and laboratory tests can help mitigate complications.
- Optimal Hemostasis During Surgery: Ensuring meticulous attention to bleeding control during the operation, including the use of hemostatic agents, sutures, and ligatures, can significantly reduce the risk of postsurgical bleeding.
- Postoperative Monitoring: Continuous monitoring of vital signs, hematocrit levels, and surgical site conditions in the immediate postoperative period allows for early detection and intervention.
Postsurgical hemorrhage remains a significant challenge in the surgical recovery process. Understanding its causes, early detection, and prompt management are essential to reducing complications and improving patient outcomes. By utilizing appropriate diagnostic methods, timely interventions, and preventive strategies, healthcare providers can mitigate the risks associated with postsurgical hemorrhage and support optimal recovery for surgical patients.