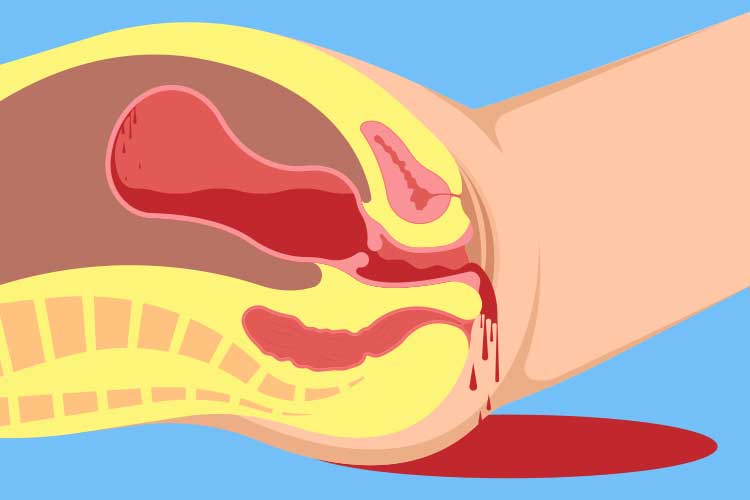
Postpartum hemorrhage (PPH) is a major obstetric emergency and the leading cause of maternal mortality worldwide. Defined as blood loss of ≥500 mL after vaginal delivery or ≥1000 mL after cesarean section, PPH requires swift identification and intervention. Its effective management is central to safe childbirth practices and maternal health preservation.
Classification of Postpartum Hemorrhage
Primary vs. Secondary PPH
- Primary PPH: Occurs within the first 24 hours post-delivery
- Secondary PPH: Occurs between 24 hours and 12 weeks postpartum
Etiological Framework: The “4 T’s” of Postpartum Hemorrhage
1. Tone – Uterine Atony
The most common cause, responsible for approximately 70–80% of PPH cases. Failure of the uterus to contract effectively leads to continuous bleeding.
2. Trauma – Genital Tract Lacerations
Includes tears of the cervix, vagina, perineum, or uterine rupture. Often missed during initial evaluation.
3. Tissue – Retained Placental Fragments
Incomplete expulsion of the placenta or membranes hinders uterine contraction and contributes to ongoing hemorrhage.
4. Thrombin – Coagulopathy
Includes preexisting or acquired disorders affecting clot formation, such as DIC or HELLP syndrome.
Risk Factors for Postpartum Hemorrhage
- Prolonged or rapid labor
- Overdistended uterus (multiple gestation, polyhydramnios)
- Use of uterine relaxants
- Previous history of PPH
- Operative delivery (forceps/vacuum)
- Placenta previa or accreta
- Infections or chorioamnionitis
Clinical Presentation and Recognition
Observable Signs:
- Heavy vaginal bleeding
- Hypotension and tachycardia
- Pallor, dizziness, altered consciousness
- Uterine fundus soft and boggy (in atony)
Quantifying Blood Loss:
Visual estimation is often inaccurate. Objective tools like gravimetric methods and calibrated drapes are recommended.
Diagnostic Measures and Investigations
- Complete Blood Count (CBC): Hemoglobin and hematocrit levels
- Coagulation Profile: PT, aPTT, fibrinogen
- Blood Typing and Crossmatching: For transfusion readiness
- Ultrasound: To detect retained placental tissue or hematomas
Pharmacologic Management
First-Line Uterotonics:
- Oxytocin: 10–40 IU in 1L NS or LR IV infusion
- Methylergometrine: 0.2 mg IM (contraindicated in hypertension)
- Carboprost (15-methyl PGF2α): 250 mcg IM every 15–90 min (max 8 doses)
- Misoprostol: 800–1000 mcg rectally or sublingually
Surgical and Interventional Management
Conservative Surgical Techniques:
- Uterine Balloon Tamponade (Bakri Balloon)
- Uterine Compression Sutures (e.g., B-Lynch)
- Uterine Artery Ligation or Uterine Artery Embolization
Definitive Surgery:
- Hysterectomy: Last resort in cases of intractable bleeding or placenta accreta spectrum
Blood and Fluid Replacement
- Crystalloids: Initial resuscitation with normal saline or Ringer’s lactate
- Blood Products:
- PRBCs for volume replacement
- FFP, Platelets, and Cryoprecipitate based on coagulation profile
- Tranexamic acid (1g IV) early administration reduces mortality
Prevention of Postpartum Hemorrhage
Active Management of Third Stage of Labor (AMTSL)
- Immediate oxytocin administration after delivery
- Controlled cord traction
- Uterine massage post-delivery
Risk Assessment Tools:
- Antenatal risk factor evaluation
- Individualized labor plans for high-risk pregnancies
- Availability of blood and emergency kits
Global Burden and Public Health Impact
- PPH accounts for nearly 25% of maternal deaths globally
- Highest incidence in low-resource settings due to delayed recognition and lack of interventions
- Investment in training, protocols, and access to care dramatically reduces maternal mortality
Long-Term Sequelae of Severe Postpartum Hemorrhage
- Sheehan’s Syndrome (postpartum hypopituitarism)
- Chronic anemia
- Psychological trauma and postnatal depression
- Loss of fertility following hysterectomy
Postpartum hemorrhage is a critical, yet manageable, obstetric complication. A thorough understanding of its etiology, prompt recognition, and adherence to structured treatment algorithms significantly improve maternal outcomes. Emphasizing prevention through AMTSL, preparedness, and skill-based training remains essential to reduce the global burden of maternal death.