Postpartum endomyometritis is a severe uterine infection occurring after childbirth, often associated with ascending bacterial contamination. Among the pathogenic organisms responsible, Streptococcus species, particularly Group A Streptococcus (Streptococcus pyogenes) and Group B Streptococcus (Streptococcus agalactiae), are significant contributors to postpartum morbidity and mortality. Understanding the pathophysiology, clinical presentation, and evidence-based treatment protocols is essential for obstetricians and infectious disease specialists.
Pathogenesis and Microbiology of Streptococcal Endomyometritis
Group A Streptococcus (GAS) and Group B Streptococcus (GBS)
GAS, though less common, leads to highly virulent infections with rapid onset and severe systemic effects. GBS is more frequently associated with subacute presentations but still poses serious risks when left untreated.
Mechanism of Infection:
- During labor and delivery, disruptions in the cervical barrier allow endogenous flora, including Streptococcus spp., to ascend into the uterine cavity.
- GAS can produce exotoxins, such as streptolysin O and streptococcal pyrogenic exotoxins, that lead to systemic inflammatory response syndrome (SIRS) and septic shock.
- GBS colonization in the genital tract increases the risk for postpartum uterine infection.
Risk Factors Associated with Streptococcal Endomyometritis
- Prolonged labor
- Premature rupture of membranes
- Cesarean section (especially without prophylactic antibiotics)
- Manual removal of the placenta
- Presence of chorioamnionitis
- Poor perineal hygiene postpartum
- Maternal immunosuppression
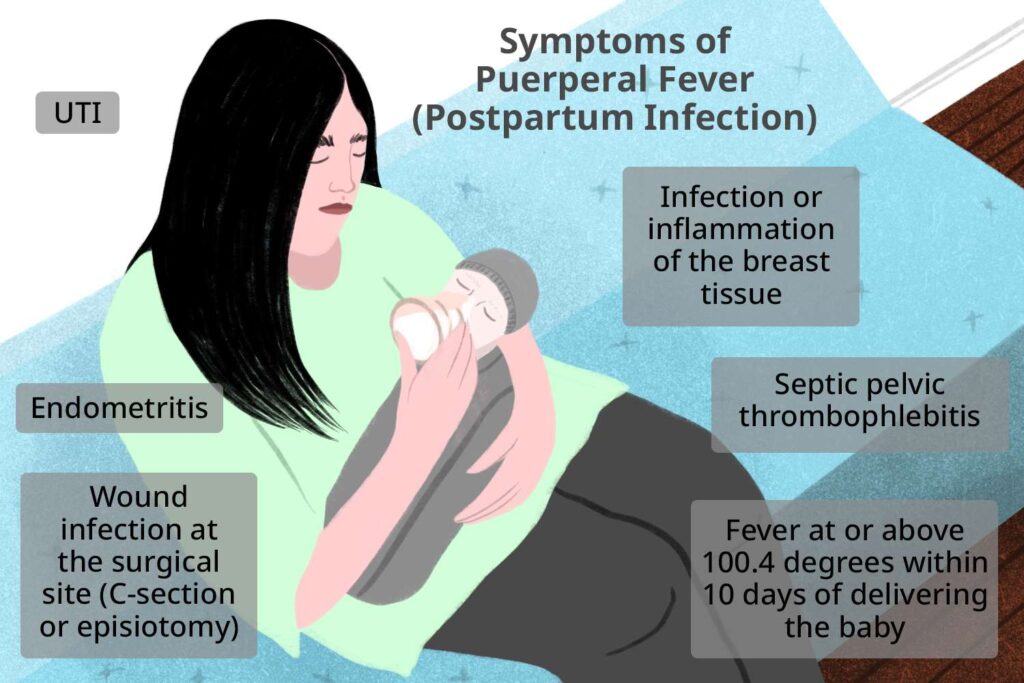
Clinical Presentation of Streptococcal Endomyometritis
Typical Symptoms:
- High-grade fever (>38°C)
- Lower abdominal pain and uterine tenderness
- Foul-smelling lochia
- Malaise, chills, and rigors
- Tachycardia and hypotension in severe cases
Advanced Complications:
- Bacteremia
- Septic pelvic thrombophlebitis
- Septic shock
- Disseminated intravascular coagulation (DIC)
Diagnostic Approach for Postpartum Endomyometritis
Laboratory Investigations:
- CBC: Elevated white blood cell count with left shift
- Blood cultures: To identify Streptococcus pyogenes or agalactiae
- Endometrial cultures: Collected using sterile aspiration techniques
- CRP and ESR: Elevated levels indicate systemic inflammation
Imaging:
- Transvaginal or transabdominal ultrasound to rule out retained products of conception and abscess formation.
Management and Treatment Strategies
Empirical Antibiotic Therapy
Empirical treatment should begin immediately upon clinical suspicion and later tailored based on culture results.
Add Ampicillin if Enterococcus is suspected.
Duration of Therapy:
- Typically 10–14 days or until the patient remains afebrile for 48 hours.
Surgical Intervention:
- Required in cases of retained placental tissue, abscesses, or uterine necrosis.
- Hysterectomy may be necessary in fulminant cases of GAS with refractory septic shock.
Prevention of Streptococcal Postpartum Infections
- Intrapartum antibiotic prophylaxis for GBS-colonized mothers
- Aseptic delivery techniques
- Cesarean section antibiotic prophylaxis administered pre-incision
- Early removal of retained placental fragments
Clinical Outcomes and Prognosis
Prognosis:
With timely diagnosis and aggressive antibiotic therapy, the prognosis is favorable. However, GAS infections can escalate rapidly, resulting in multi-organ failure and maternal death if untreated.
Complication Rates:
- Bacteremia: 15–30%
- Septic shock in GAS: ~50% mortality if delayed
Epidemiological Insights
- Incidence of postpartum endomyometritis is 1–3% after vaginal delivery and up to 27% after cesarean without antibiotic prophylaxis.
- GAS accounts for fewer than 5% of cases but is responsible for the majority of severe outcomes and maternal deaths.
Streptococcal postpartum endomyometritis remains a life-threatening complication that demands prompt recognition and aggressive management. With evolving clinical practices and adherence to preventive measures, the incidence of severe outcomes can be significantly reduced. Emphasizing early diagnosis and immediate broad-spectrum antibiotic therapy is critical in ensuring maternal survival and recovery.