Postpartum endomyometritis due to Porphyromonas species is a significant obstetric complication involving anaerobic bacterial invasion of the endometrium and myometrium. These infections, predominantly arising after cesarean section or complicated vaginal births, are associated with severe pelvic inflammation, systemic symptoms, and increased maternal morbidity if not rapidly identified and treated.
The Pathogenic Role of Porphyromonas in Postpartum Uterine Infections
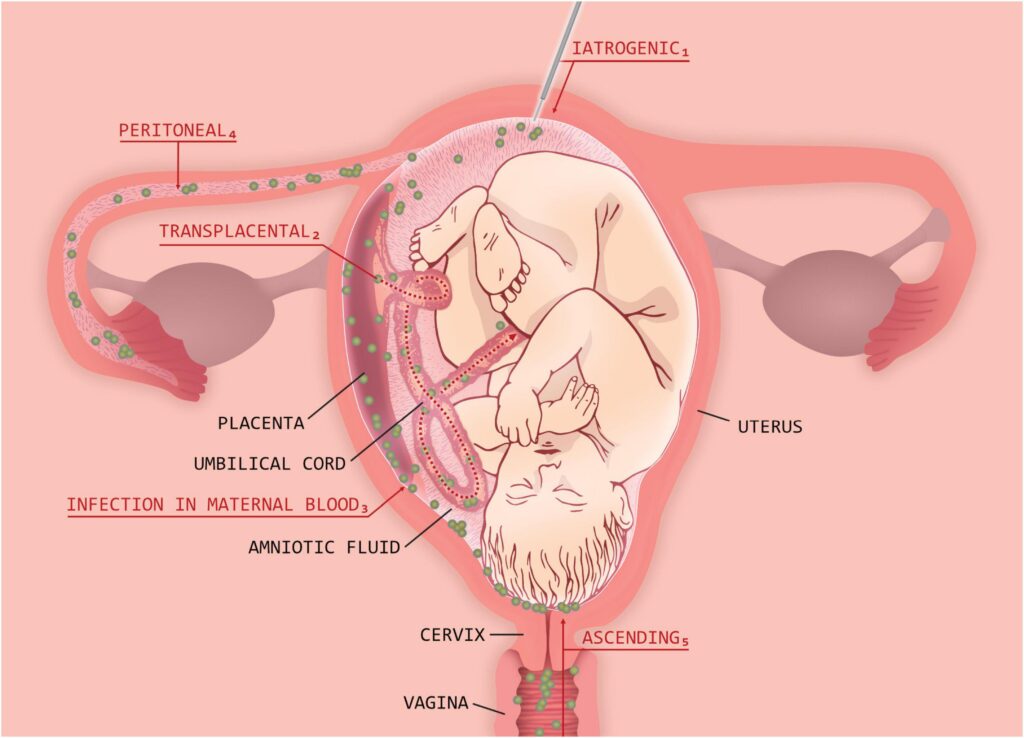
Porphyromonas spp., especially Porphyromonas asaccharolytica and Porphyromonas gingivalis, are gram-negative, obligate anaerobic bacilli that inhabit mucosal surfaces. Though typically associated with periodontal disease, these bacteria have also been isolated in obstetric and gynecologic infections due to their capacity for tissue invasion under anaerobic conditions.
These organisms flourish in environments with necrotic tissue and low oxygen tension—conditions often present in the postpartum uterus following surgical intervention, retained placental tissue, or extensive endometrial trauma.
Risk Factors for Porphyromonas-Associated Postpartum Endomyometritis
Understanding and identifying risk factors for anaerobic uterine infections allows for earlier intervention:
- Cesarean delivery without prophylactic antibiotics
- Manual removal of placenta
- Prolonged labor or rupture of membranes (>18 hours)
- Intrauterine device or catheter placement postpartum
- Multiple vaginal examinations during labor
- Retained products of conception
- Bacterial vaginosis or abnormal vaginal flora colonization
- Obesity and poor glycemic control
Clinical Presentation of Porphyromonas-Induced Endomyometritis
Symptoms typically present within the first week postpartum, with variable severity depending on the extent of infection:
- Persistent fever >38.0°C (100.4°F)
- Malodorous, purulent lochia
- Tender, subinvoluted uterus
- Pelvic and lower abdominal pain
- Tachycardia and fatigue
- Chills and rigors
- Signs of systemic inflammatory response or sepsis
In advanced stages, pelvic abscess, parametritis, or bacteremia may occur.
Diagnostic Workup for Porphyromonas-Related Endomyometritis
Clinical Evaluation
Initial diagnosis relies on history, clinical presentation, and exclusion of other causes such as urinary tract infections or wound infections.
Laboratory Testing
- CBC: Elevated white cell count with left shift
- Inflammatory markers: Raised CRP and ESR
- Blood cultures: Indicated for febrile patients with systemic symptoms
- Endometrial/vaginal cultures: Anaerobic-specific transport required for isolation of Porphyromonas
- Molecular diagnostics (PCR): Enhance detection sensitivity of anaerobic pathogens
Imaging Studies
- Transvaginal ultrasound: To detect retained tissue, gas formation, or fluid collection in the uterus
- CT/MRI pelvis: Reserved for suspected abscess, extensive pelvic involvement, or failure to respond to therapy
Antibiotic Management of Porphyromonas Endomyometritis
Anaerobic bacteria such as Porphyromonas are often resistant to first-generation cephalosporins. Timely empirical therapy followed by culture-guided adjustment is essential.
Empiric Antibiotic Therapy
- Clindamycin + Gentamicin: Preferred initial regimen due to reliable anaerobic and gram-negative coverage
- Ampicillin-Sulbactam: Effective against Porphyromonas spp.
- Piperacillin-Tazobactam or Carbapenems: For severe, polymicrobial infections or resistance concern
Targeted Therapy
Upon culture confirmation of Porphyromonas, options include:
- Metronidazole: Excellent anaerobic coverage
- Clindamycin: Alternative where metronidazole is contraindicated
- Moxifloxacin: In outpatient cases with known sensitivities
Treatment typically spans 10–14 days, extending based on clinical response and complications.
Surgical and Adjunctive Interventions
Infections unresponsive to antibiotics or associated with abscesses may necessitate:
- Evacuation of retained products via D&C
- Percutaneous or surgical drainage of pelvic abscess
- Exploratory laparotomy in cases of diffuse peritonitis
- Hysterectomy: Rare, last-resort in fulminant, unresponsive infections
Supportive care, including IV hydration, antipyretics, analgesics, and close inpatient monitoring, is vital during the acute phase.
Preventive Measures Against Porphyromonas Endomyometritis
Intrapartum and Postpartum Prophylaxis
- Prophylactic antibiotic administration prior to cesarean (e.g., cefazolin with metronidazole in high-risk patients)
- Limiting digital exams during labor
- Prompt removal of retained placental fragments
- Sterile technique during uterine manipulation
Addressing Vaginal Flora
Pre-existing bacterial vaginosis or high anaerobic colonization rates in the genital tract should be managed prenatally with:
- Metronidazole vaginal gel
- Oral clindamycin (if indicated)
Potential Complications of Untreated Anaerobic Uterine Infections
Failure to diagnose or treat Porphyromonas infection promptly can result in:
- Pelvic abscess
- Septic pelvic thrombophlebitis
- Endometritis-associated infertility
- Uterine rupture (rare)
- Systemic sepsis and multiorgan failure
Prognosis and Maternal Outcomes
With timely diagnosis and adequate antibiotic coverage, prognosis is excellent. Most patients recover fully without long-term sequelae. Delay in management increases the risk of extended hospitalization, ICU admission, or invasive intervention.
Porphyromonas-associated postpartum endomyometritis is a serious, yet preventable and treatable condition. Early recognition, anaerobic-targeted antibiotic therapy, and adherence to aseptic delivery protocols are critical to improving maternal outcomes and minimizing complications. Effective surveillance, prompt diagnostics, and appropriate escalation of care define the cornerstone of modern obstetric infection control.