Postpartum endomyometritis due to Escherichia coli (E. coli) represents a serious and potentially life-threatening uterine infection that primarily occurs following cesarean delivery or complicated vaginal births. As a gram-negative facultative anaerobe and common gut inhabitant, E. coli becomes pathogenic when introduced into the uterine cavity during delivery. Understanding its etiology, clinical presentation, and management is crucial for reducing maternal morbidity.
Pathophysiology of E. coli-Induced Postpartum Endomyometritis
Uterine Susceptibility Post-Delivery
During childbirth, especially cesarean sections, the physical barrier of the endometrial lining is disrupted, creating an entry point for pathogens. E. coli, which commonly colonizes the rectovaginal area, may ascend and invade the uterine cavity and myometrium, causing widespread inflammation.
Risk Factors Specific to E. coli Infections
- Cesarean section, especially unplanned or emergency procedures
- Prolonged labor or rupture of membranes (>18 hours)
- Multiple vaginal examinations during labor
- Intrauterine manipulation or instrumentation
- Pre-existing genital tract colonization with E. coli
- Lack of prophylactic antibiotic use
- Obesity, diabetes, or immunocompromised state
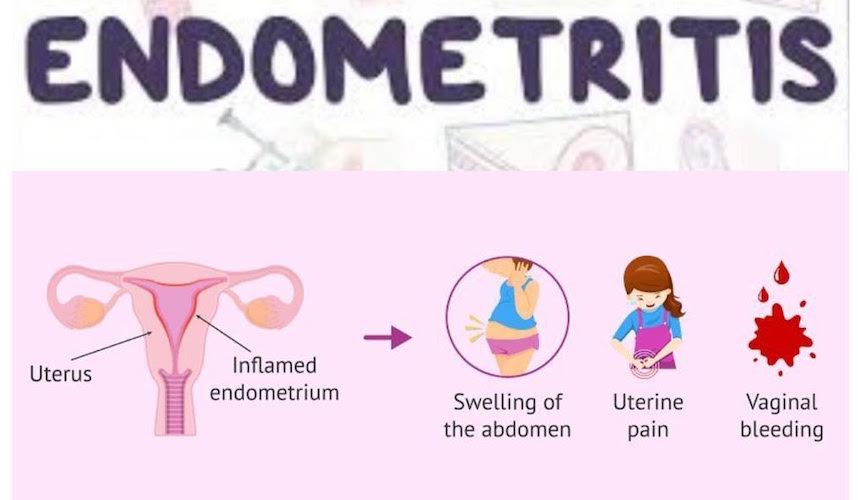
Clinical Presentation and Symptoms
Postpartum endomyometritis typically develops within the first week after delivery. The hallmark signs include:
- Persistent postpartum fever (>38°C or 100.4°F) beyond 24 hours
- Uterine tenderness, often diffuse and aggravated by palpation
- Foul-smelling or purulent lochia
- Lower abdominal or pelvic pain
- Tachycardia and malaise
- Subinvolution of the uterus on examination
- Signs of systemic infection in severe cases (e.g., hypotension, chills)
Diagnostic Approach to Postpartum Endomyometritis Due to E. coli
Clinical Assessment
Diagnosis is primarily clinical, supported by laboratory and imaging data. A history of recent childbirth combined with characteristic symptoms is often sufficient to initiate empirical therapy.
Laboratory Tests
- CBC with differential: Elevated WBC count with left shift
- C-reactive protein (CRP) and ESR: Raised inflammatory markers
- Endometrial or lochial swab culture: Confirms E. coli presence and antibiotic susceptibility
- Blood cultures: Essential if systemic symptoms or high-grade fever is present
- Urinalysis and urine culture: To rule out concurrent urinary tract infection
Imaging Studies
- Ultrasound of the pelvis: Detects retained products, fluid collections, or uterine abnormalities
- CT/MRI (rarely needed): Reserved for suspected complications such as abscess or septic thrombophlebitis
Targeted Treatment Strategies
Empirical Antimicrobial Therapy
Treatment should commence immediately after diagnosis, covering both aerobic and anaerobic pathogens until culture results are available.
Recommended IV Regimens:
- Clindamycin + Gentamicin: Broad-spectrum and standard first-line treatment
- Ampicillin + Gentamicin + Metronidazole: Alternative for extended coverage
- Piperacillin-Tazobactam or Ceftriaxone + Metronidazole: For resistant E. coli strains or severe infections
Upon identification of E. coli through cultures, antibiotics may be de-escalated based on sensitivity. Duration typically extends for 48–72 hours post-fever resolution, followed by a course of oral antibiotics for up to 7–10 days.
Supportive Measures
- IV fluids for hydration and circulatory support
- Antipyretics for fever control
- Monitoring of vital signs, WBC count, and uterine involution
Surgical and Invasive Interventions
Indicated in cases unresponsive to antibiotics or when imaging reveals complications:
- Evacuation of retained placental tissue
- Drainage of pelvic abscesses
- Hysterectomy (rare) in fulminant, refractory infections
Prevention of Postpartum E. coli Endomyometritis
Prophylactic Antibiotics
A single dose of cefazolin or ampicillin-sulbactam before cesarean delivery significantly reduces the risk of infection, including those caused by E. coli.
Labor and Delivery Best Practices
- Limit vaginal exams once membranes rupture
- Maintain sterile techniques during delivery
- Prompt delivery after membrane rupture
- Avoid unnecessary instrumentation (e.g., fetal scalp electrodes)
Complications and Long-Term Sequelae
If inadequately treated, E. coli endomyometritis can lead to:
- Pelvic abscesses
- Peritonitis
- Septic shock
- Intrauterine adhesions (Asherman syndrome)
- Secondary infertility
- Extended hospitalization and increased healthcare costs
Prognosis and Recovery
With timely diagnosis and appropriate antibiotic therapy, the prognosis is excellent. Most patients recover fully within days, with minimal risk of recurrence if predisposing factors are addressed.
Postpartum endomyometritis due to E. coli is a preventable and treatable uterine infection that necessitates prompt medical attention. Identification of risk factors, early recognition of clinical symptoms, and institution of targeted antibiotic therapy remain the cornerstones of effective management. Obstetric care teams must prioritize sterile delivery protocols and prophylactic strategies to minimize maternal complications in the postpartum period.