Postpartum endomyometritis due to Bacteroides species is a severe polymicrobial infection that affects the uterine lining and myometrial tissue following childbirth, particularly after cesarean delivery. Prompt recognition and targeted antimicrobial therapy are essential to prevent complications such as sepsis, infertility, and prolonged hospitalization.
Understanding Postpartum Endomyometritis
Postpartum endomyometritis is an ascending genital tract infection involving the endometrium and the muscular wall of the uterus (myometrium). It most commonly occurs within the first 10 days postpartum and is predominantly associated with cesarean deliveries, especially when conducted under emergency or non-sterile conditions.
Role of Bacteroides in Postpartum Infections
Overview of Bacteroides Species
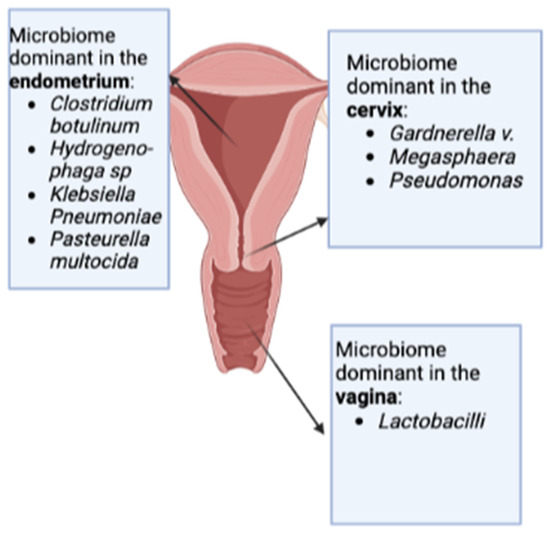
Bacteroides are gram-negative, obligate anaerobic bacteria that are part of the normal flora of the gastrointestinal and vaginal tract. While generally harmless in their natural environment, these organisms become opportunistic pathogens when introduced into sterile body sites, such as the uterine cavity during or after delivery.
Common Pathogenic Strains:
- Bacteroides fragilis
- Bacteroides vulgatus
- Bacteroides thetaiotaomicron
These bacteria produce β-lactamase and possess a polysaccharide capsule, both contributing to their virulence and resistance to certain antibiotics.
Risk Factors for Bacteroides-Related Endomyometritis
- Cesarean delivery, especially emergency procedures
- Prolonged rupture of membranes (>18 hours)
- Frequent vaginal examinations during labor
- Internal fetal monitoring devices
- Retained placental fragments or blood clots
- Pre-existing bacterial vaginosis
- Inadequate intrapartum prophylactic antibiotics
Clinical Features of Postpartum Endomyometritis
Patients typically present within the first week postpartum with:
- Fever >38°C (100.4°F) persisting beyond 24 hours postpartum
- Uterine tenderness, often midline and exacerbated by palpation
- Foul-smelling lochia or purulent vaginal discharge
- Tachycardia
- Malaise or fatigue
- Lower abdominal pain or pelvic discomfort
If left untreated, the infection can escalate to pelvic abscess, septic pelvic thrombophlebitis, or systemic sepsis.
Diagnostic Evaluation
Clinical Diagnosis
Endomyometritis is primarily diagnosed based on clinical symptoms in the context of recent childbirth. Uterine tenderness and postpartum fever are hallmark indicators.
Laboratory and Imaging Tests
- Complete Blood Count (CBC): Elevated white blood cell count with neutrophilia
- C-Reactive Protein (CRP) and ESR: Raised inflammatory markers
- Endometrial or lochial cultures: May isolate Bacteroides or other anaerobic flora
- Blood cultures: Essential in febrile or hemodynamically unstable patients
- Ultrasound: To detect retained products of conception or intrauterine fluid collections
- CT scan: Reserved for complicated cases or suspected pelvic abscess
Antimicrobial Therapy and Clinical Management
Empirical Antibiotic Treatment
Due to the polymicrobial nature of the infection, broad-spectrum antibiotics covering anaerobes, aerobes, and gram-negative organisms are indicated.
Preferred Regimens:
- Clindamycin + Gentamicin: Widely used and highly effective
- Ampicillin + Gentamicin + Metronidazole: Alternative in more severe infections
- Extended-spectrum beta-lactams: Such as piperacillin-tazobactam or a carbapenem, in resistant cases
Duration:
Treatment generally continues for 24–48 hours after symptom resolution, followed by oral antibiotics for 7–10 days if necessary.
Surgical Intervention
Required in cases with:
- Retained placental tissue
- Uterine abscess or necrosis
- Lack of response to antimicrobial therapy
Preventive Strategies in High-Risk Deliveries
Prophylactic Antibiotics
- Administering a single dose of IV cefazolin or clindamycin before skin incision during cesarean delivery significantly reduces infection rates.
Sterile Technique and Minimizing Invasive Procedures
- Limit the number of vaginal examinations during labor
- Avoid unnecessary use of internal monitors
- Prompt delivery once membranes are ruptured
Maternal and Neonatal Outcomes
With early diagnosis and proper treatment, recovery is typically complete. However, delayed treatment can lead to serious complications:
Maternal Risks
- Pelvic peritonitis
- Septic shock
- Infertility due to intrauterine adhesions (Asherman syndrome)
Neonatal Risks (Indirect)
- Separation from mother due to prolonged hospitalization
- Impaired breastfeeding and bonding
Postpartum endomyometritis due to Bacteroides species remains a significant cause of puerperal morbidity, particularly after cesarean delivery. Recognizing the signs early, understanding the microbial etiology, and initiating targeted antibiotic therapy are critical to minimizing maternal complications. Emphasis on prophylaxis and safe obstetric practices can effectively reduce incidence and ensure safer postpartum outcomes.