Postoperative ileus (POI) is a temporary impairment of gastrointestinal (GI) motility following surgical procedures, particularly abdominal surgeries. It is a common yet complex complication that delays bowel function recovery, prolongs hospitalization, increases healthcare costs, and negatively impacts patient outcomes. Recognizing its risk factors, clinical presentation, and effective interventions is essential to enhance recovery and reduce associated morbidity.
Pathophysiology and Causes of Postoperative Ileus
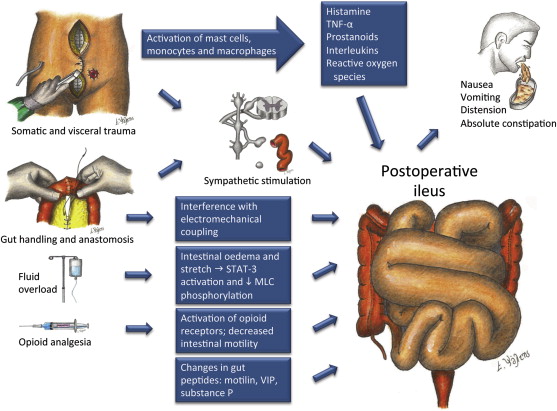
POI results from a combination of neurogenic, inflammatory, and pharmacologic factors that disrupt coordinated intestinal motility.
Neurogenic Disruption
Surgical stress activates sympathetic neural pathways, which inhibit parasympathetic activity responsible for gut peristalsis. This autonomic imbalance contributes to intestinal atony.
Inflammatory Cascade
Surgical manipulation of the bowel triggers an inflammatory response involving macrophage activation, cytokine release (e.g., IL-6, TNF-α), and infiltration of leukocytes into the intestinal muscularis. These changes suppress smooth muscle contractions.
Pharmacologic Influences
Opioid analgesics, commonly administered for postoperative pain, bind to μ-opioid receptors in the gut, slowing motility and contributing significantly to ileus development.
Clinical Presentation and Diagnosis
Symptoms of Postoperative Ileus
- Abdominal distension
- Bloating and discomfort
- Delayed passage of flatus or stool
- Nausea and vomiting
- Hypoactive or absent bowel sounds
Symptoms typically manifest within 24–72 hours after surgery and may last several days depending on severity.
Diagnostic Criteria
Diagnosis is clinical, supported by imaging when complications are suspected. Key findings include:
- Abdominal X-rays: Dilated bowel loops without transition point
- CT scans: Exclusion of mechanical obstruction or abscess
- Physical exam: Tympanic abdomen, reduced bowel sounds
Differentiation from mechanical bowel obstruction is critical, as management strategies differ substantially.
Classification of Ileus Duration
| Type | Duration | Implications |
|---|---|---|
| Physiologic Ileus | <3 days (small bowel), <5 days (colon) | Normal postoperative response |
| Pathologic Ileus | >3–5 days | Indicates complications or ineffective management |
Risk Factors for Postoperative Ileus
- Abdominal or pelvic surgery (especially colorectal)
- Extensive bowel manipulation
- Opioid use
- Electrolyte imbalances (e.g., hypokalemia, hyponatremia)
- Peritonitis or intra-abdominal sepsis
- Advanced age and comorbid conditions (e.g., diabetes)
Multimodal Strategies for Management
Effective POI management involves combining pharmacologic and non-pharmacologic approaches to promote early GI recovery.
Enhanced Recovery After Surgery (ERAS) Protocols
ERAS guidelines promote early mobilization, reduced opioid use, and early enteral nutrition to mitigate POI risk. Key components include:
- Preoperative counseling
- Avoidance of prolonged fasting
- Intraoperative fluid management
- Minimally invasive surgical techniques
Pharmacologic Interventions
1. Opioid-Sparing Analgesia
- NSAIDs and acetaminophen: Reduce inflammation and pain without GI motility suppression.
- Regional anesthesia (e.g., epidural): Provides effective pain relief while reducing opioid use.
2. Prokinetic Agents
- Alvimopan: A selective μ-opioid receptor antagonist that accelerates GI recovery in patients undergoing bowel resection.
- Metoclopramide and erythromycin: Occasionally used but with limited efficacy in POI.
3. Laxatives and Enemas
Used cautiously to stimulate bowel movement, though their use in true POI remains controversial due to risk of bowel injury.
Non-Pharmacologic Management
Early Ambulation
Mobilizing patients within 24 hours of surgery stimulates autonomic function and improves intestinal motility.
Chewing Gum
Chewing gum mimics food intake by stimulating vagal tone and enhancing salivary and GI hormone release, thereby improving bowel recovery.
Early Enteral Feeding
Initiating oral or enteral nutrition as early as tolerated promotes peristalsis, reduces infection risk, and improves healing.
Complications and Long-Term Implications
If unrecognized or poorly managed, POI may lead to:
- Prolonged hospitalization
- Increased risk of nosocomial infections
- Nutritional deficiencies
- Higher healthcare costs
- Transition to chronic pseudo-obstruction in rare cases
Timely identification and adherence to ERAS principles are essential for reducing these complications.
Prevention of Postoperative Ileus: Evidence-Based Approaches
- Minimally invasive surgery (laparoscopy): Associated with less bowel manipulation and quicker recovery.
- Avoidance of routine nasogastric tubes: Their use delays oral intake and prolongs ileus.
- Perioperative fluid restriction: Prevents bowel edema and reduces ileus duration.
- Prehabilitation: Improves postoperative outcomes through nutritional and physical optimization before surgery.
Postoperative ileus remains a multifactorial and preventable complication of surgical care. Implementing evidence-based strategies, including ERAS protocols, opioid-sparing analgesia, early mobilization, and targeted pharmacologic agents, is critical to minimizing its incidence and severity. Through a structured and individualized approach, healthcare providers can ensure faster recovery, lower morbidity, and improved patient outcomes.