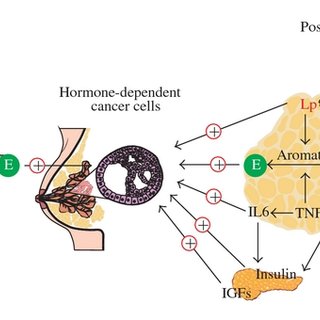
Hormone-dependent breast cancer, also referred to as hormone receptor-positive (HR+) breast cancer, is characterized by the expression of estrogen receptors (ER) and/or progesterone receptors (PR) on tumor cells. In postmenopausal women, systemic estrogen levels decline significantly; however, local estrogen production in adipose tissues continues to stimulate cancer growth in ER+ tumors. Effective adjunct (adjuvant) treatments play a critical role in reducing the risk of recurrence and improving survival outcomes.
Hormone Receptor Status and Its Therapeutic Implications
Understanding hormone receptor status is essential to guide treatment:
- ER+/PR+ tumors respond favorably to endocrine therapy.
- HER2 status also influences adjunct treatment selection.
- Triple-positive tumors (ER+/PR+/HER2+) may require combination regimens.
Molecular profiling further refines risk stratification and aids in tailoring individualized therapy plans.
Endocrine Therapy as the Foundation of Adjunct Treatment
Endocrine therapy remains the cornerstone of adjuvant treatment for postmenopausal hormone-dependent breast cancer. It acts by reducing estrogen stimulation of cancer cells through either estrogen suppression or estrogen receptor blockade.
Aromatase Inhibitors (AIs)
AIs are preferred in postmenopausal women due to their mechanism of action:
- Letrozole, Anastrozole, and Exemestane inhibit the aromatase enzyme, reducing peripheral conversion of androgens to estrogens.
- AIs are associated with superior disease-free survival compared to tamoxifen in large-scale trials such as ATAC and BIG 1-98.
Selective Estrogen Receptor Modulators (SERMs)
- Tamoxifen competitively inhibits estrogen binding to receptors in breast tissue.
- Commonly used in patients intolerant to AIs or in sequential therapy following AI courses.
Treatment Duration and Sequencing
- Standard endocrine therapy duration is 5–10 years, with various sequencing strategies:
- Initial 5 years of AIs
- Tamoxifen for 2–3 years followed by AIs for 2–3 years
- Extended therapy for high-risk recurrence cases
Chemotherapy Considerations in High-Risk Hormone-Dependent Cases
While endocrine therapy is primary, chemotherapy is considered for:
- High tumor grade
- Lymph node involvement
- High-risk genomic profiles (e.g., Oncotype DX Recurrence Score)
Common regimens include anthracycline- and taxane-based combinations. Integration with endocrine therapy is sequential to avoid treatment overlap.
Targeted Therapy for HER2-Positive Subtype
For patients with HER2-positive, hormone receptor-positive breast cancer:
- Trastuzumab (Herceptin) is administered concurrently with chemotherapy, followed by maintenance for one year.
- Pertuzumab, neratinib, and trastuzumab-emtansine (T-DM1) are used in select high-risk or metastatic settings.
- Dual targeting with HER2 blockade and endocrine therapy provides survival benefits.
Bone Health and Estrogen Deprivation: Mitigation Strategies
Estrogen depletion via AIs leads to accelerated bone loss, increasing fracture risk. Adjunct strategies include:
- Bisphosphonates (e.g., zoledronic acid) and Denosumab to improve bone mineral density and reduce skeletal-related events
- Regular DEXA scans to monitor bone health
- Calcium and vitamin D supplementation
Side Effect Management and Patient Quality of Life
Long-term adherence is critical, but treatment can pose challenges:
- Aromatase inhibitors: Joint pain, bone loss, cardiovascular effects
- Tamoxifen: Risk of thromboembolism, endometrial cancer
- Supportive care includes physical therapy, lifestyle modification, and psychological support
Comprehensive management improves tolerability and compliance.
Genomic Assays and Precision in Adjunct Therapy Planning
Molecular assays offer predictive and prognostic value:
- Oncotype DX: Guides chemotherapy benefit in ER+, HER2−, node-negative disease
- Prosigna (PAM50) and EndoPredict: Identify patients likely to benefit from extended endocrine therapy
Incorporation of genomic data ensures precision in treatment decisions.
Survivorship and Long-Term Follow-Up
Adjunct therapy improves long-term outcomes, but ongoing surveillance is essential:
- Annual mammograms
- Regular gynecologic exams (especially in tamoxifen users)
- Cardiovascular monitoring for AI and HER2 therapies
- Management of menopausal symptoms and psychosocial well-being
A multidisciplinary approach supports survivorship quality.
Adjunct treatment for postmenopausal hormone-dependent breast cancer is a dynamic field, grounded in personalized endocrine therapy, selective chemotherapy use, and targeted biological agents. Optimization of these therapies, informed by risk stratification and molecular profiling, leads to improved disease control and survival. Structured follow-up and holistic support ensure adherence, minimize complications, and enhance the patient journey from diagnosis to long-term remission.