Post-operative nausea and vomiting (PONV) is a frequent complication following anesthesia and surgery, affecting up to 30% of all surgical patients and up to 80% of high-risk individuals. This condition can significantly impact patient comfort, prolong recovery, and increase healthcare costs due to delayed discharge or unplanned hospital admission. A multidisciplinary approach to risk assessment, prophylaxis, and treatment is crucial for optimal patient outcomes.
Primary Causes of PONV
1. Anesthetic Agents
Volatile anesthetics (e.g., sevoflurane, desflurane) and nitrous oxide are strongly associated with increased PONV risk. Opioids used intraoperatively or postoperatively further heighten susceptibility.
2. Surgical Procedures
Surgeries with longer duration or involving intra-abdominal, laparoscopic, gynecological, or ENT areas are more likely to trigger nausea and vomiting postoperatively.
3. Patient-Related Risk Factors
- Female gender
- Non-smoking status
- History of motion sickness or prior PONV
- Younger age (especially under 50)
- Use of postoperative opioids
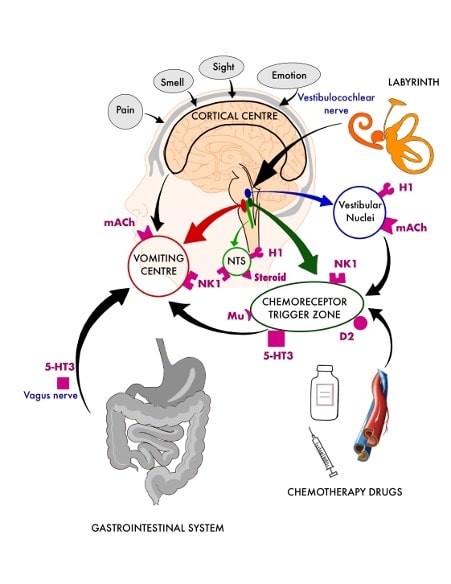
4. Physiological Mechanisms
PONV is mediated by neurotransmitters such as dopamine, serotonin (5-HT3), histamine, acetylcholine, and neurokinin-1, which activate the vomiting center via the chemoreceptor trigger zone (CTZ) in the medulla.
Risk Assessment Tools for PONV
Apfel Simplified Risk Score
This widely adopted tool assigns 1 point for each of the following:
- Female gender
- History of PONV or motion sickness
- Non-smoker
- Postoperative opioid use
Risk Stratification:
- 0–1 points: Low risk (~10%)
- 2 points: Moderate risk (~40%)
- 3–4 points: High risk (60–80%)
This predictive model aids in selecting appropriate prophylactic and therapeutic interventions.
Effective Prevention Strategies
1. Pharmacologic Prophylaxis
Combination therapy is more effective than monotherapy for moderate-to-high-risk patients.
| Class | Example Agents | Mechanism of Action |
|---|---|---|
| 5-HT3 Antagonists | Ondansetron, Palonosetron | Block serotonin receptors in CTZ |
| Dopamine Antagonists | Droperidol, Metoclopramide | Block dopamine receptors |
| NK1 Antagonists | Aprepitant | Block neurokinin-1 receptors |
| Antihistamines | Dimenhydrinate | Block histamine receptors |
| Anticholinergics | Scopolamine patch | Inhibit muscarinic receptors |
2. Anesthesia Modifications
- Use of total intravenous anesthesia (TIVA) with propofol
- Minimizing or avoiding volatile anesthetics and nitrous oxide
- Limiting intraoperative and postoperative opioids with multimodal analgesia
3. Non-Pharmacologic Measures
- Adequate hydration with IV fluids
- Acupuncture or acupressure at P6 (Neiguan) point
- Avoidance of sudden position changes post-surgery
Management of Established PONV
Treatment should involve an agent from a different drug class than that used for prophylaxis. For example, if a 5-HT3 antagonist was used preemptively, a dopamine antagonist or NK1 antagonist may be considered.
Acute Management Options:
- Ondansetron 4 mg IV
- Metoclopramide 10 mg IV
- Dexamethasone 4–8 mg IV
- Droperidol 0.625–1.25 mg IV (monitor for QT prolongation)
In cases of persistent or refractory PONV, a stepwise escalation strategy is essential.
Special Populations and Considerations
Pediatric Patients
Children aged 3 and above are susceptible to PONV, particularly in strabismus or tonsillectomy procedures. Weight-based dosing of ondansetron or dexamethasone is recommended.
Elderly Patients
Although less prone to PONV, careful drug selection is required due to altered pharmacodynamics and comorbidity profiles.
Outpatient Surgery
Quick onset, short-acting antiemetics are preferred. Prophylaxis enhances early discharge and recovery metrics.
Post-Discharge Nausea and Vomiting (PDNV)
Up to 37% of patients may experience nausea and vomiting after discharge, particularly following outpatient procedures. Extended-release formulations or longer-acting agents like palonosetron can provide continued relief.
Key Takeaways and Best Practices
- Multimodal prophylaxis is the cornerstone of effective PONV prevention in high-risk individuals.
- Tailored treatment should align with individual risk profiles and surgical/anesthetic context.
- Utilize risk prediction tools to guide evidence-based prophylaxis.
- Prioritize opioid-sparing analgesia and non-pharmacologic adjuncts.
- Implement stepwise rescue therapy for breakthrough or persistent symptoms.
Post-operative nausea and vomiting remains a significant challenge in perioperative care. With an evidence-based, patient-centered approach involving risk stratification, proactive prophylaxis, and individualized treatment, we can dramatically improve patient recovery, comfort, and surgical outcomes.