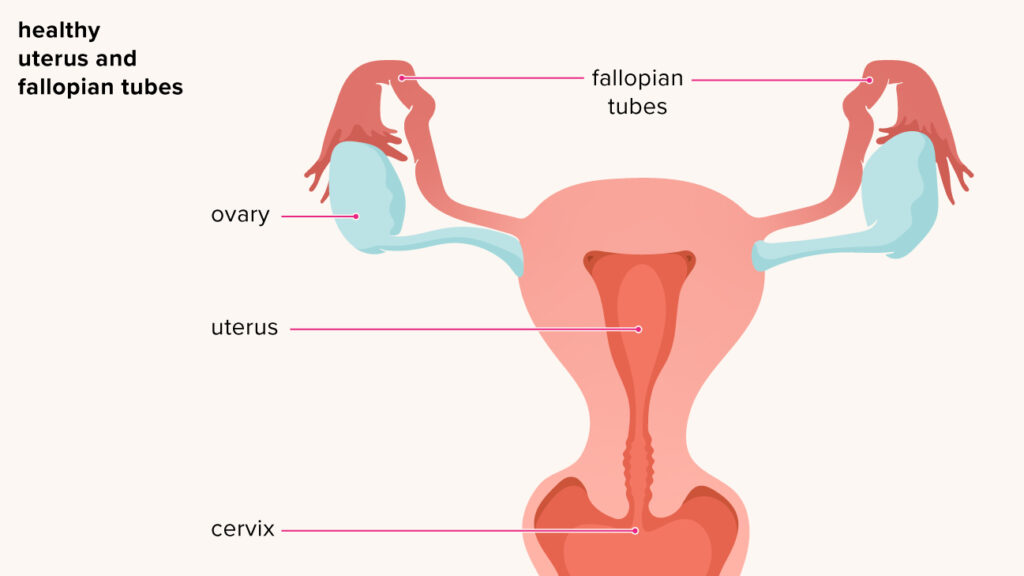
Peptostreptococcus species are obligate anaerobic, Gram-positive cocci that are part of the normal flora in the vagina, gastrointestinal tract, and oral cavity. Despite their commensal status, these organisms can become pathogenic under surgical conditions. In gynecological surgeries, particularly those involving the uterus and adnexa, Peptostreptococcus may translocate into sterile areas, resulting in polymicrobial infections. It is a prominent anaerobe implicated in pelvic abscesses, postoperative endometritis, tubo-ovarian abscesses, and pelvic cellulitis.
Pathogenesis: How Peptostreptococcus Causes Infection After Gynecologic Surgery
The pathogenesis of Peptostreptococcus infections lies in their ability to thrive in low oxygen environments, such as necrotic tissue or poorly perfused surgical sites. These bacteria often act synergistically with other anaerobes or facultative aerobes (e.g., E. coli, Bacteroides fragilis) to enhance virulence.
Virulence Characteristics:
- Adhesion to host epithelium and biomaterials
- Enzymatic degradation of tissue barriers
- Synergism with aerobic bacteria, increasing resistance to phagocytosis
- Ability to form abscesses with a fibrous capsule that resists antibiotic penetration
The anaerobic environment post-surgery—especially when hematomas, necrosis, or devitalized tissue are present—provides ideal conditions for infection.
Risk Factors for Peptostreptococcal Infections After Gynecological Surgery
Postoperative infection due to Peptostreptococcus is more likely to occur when the following risk factors are present:
- Prolonged or complex pelvic surgeries
- Inadequate intraoperative antisepsis
- Presence of foreign bodies (e.g., surgical mesh, suture material)
- Tissue devascularization or necrosis
- Contamination from vaginal flora during procedures
- Diabetes, immunosuppression, or recent antibiotic use
- Inadequate anaerobic coverage in prophylactic antibiotics
Clinical Presentation of Postoperative Peptostreptococcus Infection
Typical Signs and Symptoms:
- High-grade fever typically manifesting 2–5 days post-surgery
- Lower abdominal and pelvic pain unresponsive to standard analgesia
- Foul-smelling vaginal discharge with anaerobic characteristics
- Localized signs of abscess such as swelling, tenderness, or induration
- Signs of systemic infection, including fatigue, nausea, and chills
- Tachycardia or hypotension, especially in advancing cases of septicemia
Clinical signs may be subtle early on due to the indolent nature of anaerobic infections, emphasizing the need for prompt clinical assessment.
Diagnostic Workup for Suspected Peptostreptococcal Infections
Laboratory Studies:
- CBC: Leukocytosis with left shift
- C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR): Elevated in most cases
- Anaerobic blood cultures: Essential for bacteremia diagnosis
- Pus or aspirate from abscess: Anaerobic culture and Gram stain confirm Peptostreptococcus presence
- PCR and 16S rRNA gene sequencing: Useful for identifying anaerobes not growing in culture
Imaging Studies:
- Pelvic Ultrasound: Identifies abscess formation or fluid collection
- CT scan with contrast: Gold standard for defining extent of infection and guiding drainage
- MRI pelvis: Useful in deep pelvic or soft-tissue involvement not clearly visualized on CT
Medical and Surgical Management of Postoperative Peptostreptococcal Infection
Empirical and Directed Antibiotic Therapy
Due to the polymicrobial nature of these infections, broad-spectrum anaerobic coverage is essential, followed by targeted therapy based on culture.
Initial Empirical Therapy:
- Piperacillin-tazobactam
- Cefotetan or Cefoxitin
- Clindamycin plus gentamicin
- Metronidazole with third-generation cephalosporins
Targeted Therapy for Peptostreptococcus:
- Metronidazole (excellent anaerobic coverage)
- Clindamycin (active against anaerobes, though resistance is emerging)
- Carbapenems (e.g., Meropenem for resistant strains or severe infection)
- Penicillin G in susceptible isolates
Duration typically ranges between 10–14 days but may extend to 3–4 weeks in complicated cases involving abscesses or bacteremia.
Surgical Intervention:
- Percutaneous or laparoscopic drainage of abscesses
- Surgical debridement of necrotic or infected tissues
- Removal of foreign bodies or sutures acting as nidus
- Laparotomy in severe, non-responding cases
Prognosis and Complications of Postoperative Peptostreptococcal Infections
Potential Complications:
- Pelvic abscess rupture
- Sepsis and multi-organ failure
- Pelvic thrombophlebitis
- Fistula formation (e.g., uterovaginal or rectovaginal)
- Chronic pelvic pain or infertility
- Persistent infection or recurrence
Timely diagnosis and effective antimicrobial therapy significantly reduce the risk of long-term morbidity.
Prevention Strategies in Gynecologic Surgeries
Preoperative Interventions:
- Vaginal antiseptic preparation with povidone-iodine or chlorhexidine
- Prophylactic antibiotics with anaerobic coverage before incision
- Screening and treatment of pre-existing vaginal infections
Intraoperative and Postoperative Measures:
- Strict aseptic technique during instrument handling and vaginal access
- Minimize use of foreign material unless necessary
- Early detection and management of postoperative hematomas
- Limiting catheterization and early ambulation
Frequently Asked Questions
What is Peptostreptococcus and why is it dangerous after gynecologic surgery?
It is an anaerobic bacterium part of normal vaginal flora but can cause serious infections when introduced into surgical sites, leading to abscesses or sepsis.
How soon do infections typically appear post-surgery?
Symptoms usually develop within 2–5 days but may be delayed in low-grade infections.
Can these infections be cured with antibiotics alone?
Uncomplicated cases may resolve with antibiotics, but abscesses or necrotic tissue often require surgical intervention.
What antibiotics are effective against Peptostreptococcus?
Metronidazole, Clindamycin, and beta-lactam/beta-lactamase inhibitor combinations are commonly used.
Is prevention possible in gynecologic surgeries?
Yes. Prophylactic antibiotics, sterile technique, and good postoperative care are key preventive strategies.
Postoperative gynecological infections caused by Peptostreptococcus require vigilant diagnosis, robust anaerobic coverage, and surgical management when necessary. As a silent yet potent pathogen, its role in polymicrobial pelvic infections mandates prompt clinical recognition. Comprehensive preoperative planning, timely intervention, and coordinated care can effectively reduce morbidity and enhance recovery in affected patients.