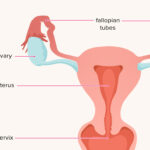
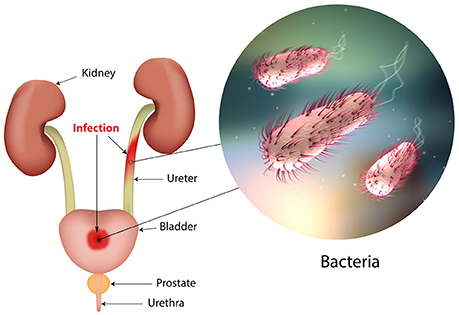
Escherichia coli (E. coli) is a common Gram-negative bacillus that resides in the lower gastrointestinal tract. While most strains are non-pathogenic in their natural habitat, their translocation during or after gynecologic procedures can lead to serious infections. E. coli is one of the most frequent bacterial pathogens isolated in post-op gynecological infections, particularly in pelvic abscesses, endometritis, and urinary tract infections following surgeries such as hysterectomy or cesarean section.
Pathophysiology: How E. coli Infects Gynecologic Surgical Sites
E. coli can access sterile pelvic organs during surgical interventions via direct contamination, translocation from adjacent structures, or hematogenous spread. Once introduced, the organism uses several virulence mechanisms:
- Fimbriae (pili) for adhesion to epithelial cells
- Lipopolysaccharide (LPS) causing inflammation and septic response
- Hemolysin production, resulting in cell lysis
- Iron-scavenging systems, supporting survival in iron-poor environments like the peritoneal cavity
- Biofilm formation on surgical materials or necrotic tissue
These factors allow E. coli to colonize, invade, and evade host defenses, ultimately causing systemic and localized infection.
Risk Factors Associated with Postoperative E. coli Infections
Patients undergoing gynecologic surgery are susceptible to postoperative infections due to E. coli when one or more of the following risk factors are present:
- Prolonged surgical duration or complex procedures
- Intraoperative bowel injury or contamination
- Indwelling urinary catheter placement
- Immunocompromised state or diabetes mellitus
- Poor perioperative aseptic technique
- Use of foreign materials (e.g., surgical mesh)
- Pre-existing bacterial vaginosis or UTI
Clinical Manifestations of E. coli Infections Post-Gynecologic Surgery
Recognizing Symptoms of E. coli-Related Infections
The clinical presentation varies based on the site and severity of infection. Common manifestations include:
- Fever (≥38.5°C) within 72 hours post-surgery
- Lower abdominal or pelvic pain
- Foul-smelling vaginal or wound discharge
- Suprapubic tenderness or costovertebral angle pain (suggestive of UTI)
- Dysuria or increased urinary frequency
- Signs of peritonitis or sepsis in severe cases
- Hemodynamic instability if bacteremia develops
A high index of suspicion is essential, especially when symptoms progress rapidly in the early postoperative period.
Diagnostic Approach to Postoperative E. coli Infections
Laboratory and Microbiologic Investigations
- Complete blood count (CBC): Elevated white blood cell count with neutrophilia
- Urinalysis and urine culture: Confirms urinary tract involvement
- Endometrial or wound swab cultures: Identifies E. coli strain and antibiotic susceptibility
- Blood cultures: Required when systemic infection or sepsis is suspected
- C-reactive protein (CRP) and procalcitonin: Useful markers for inflammation and bacterial load
Radiologic Evaluation
- Pelvic ultrasound: Detects fluid collections, abscesses, or hematomas
- Contrast-enhanced CT scan: Offers detailed visualization of pelvic and retroperitoneal structures
- MRI pelvis: Reserved for complex or recurrent infections
Therapeutic Management of E. coli Postoperative Infections
Empirical and Targeted Antibiotic Therapy
Initiating early empirical therapy is crucial, followed by tailoring the treatment based on culture sensitivity results.
Empirical Regimens:
- Piperacillin-tazobactam
- Ceftriaxone + Metronidazole
- Ertapenem (in cases with ESBL-producing E. coli suspicion)
Targeted Antibiotics:
- E. coli (non-ESBL): Cefotaxime, Ciprofloxacin, Amoxicillin-clavulanate
- ESBL-producing E. coli: Carbapenems (Meropenem, Imipenem)
- Multi-drug resistant strains: Colistin or Fosfomycin, based on MIC values
Duration of treatment generally ranges from 7 to 14 days, adjusted per severity and clinical response.
Surgical Intervention and Supportive Care
- Drainage of abscesses: Via image-guided aspiration or laparoscopic approach
- Debridement of necrotic tissue or infected mesh
- IV fluids and electrolyte correction in cases of systemic illness
- Hemodynamic support and ICU admission for patients with septic shock
Prevention of E. coli Infections in Gynecologic Surgeries
Preoperative Measures
- Routine screening for urinary tract infection and treating prior to surgery
- Administering appropriate preoperative prophylactic antibiotics
- Strict bowel preparation protocols in colorectal or combined pelvic procedures
- Maintaining sterile conditions during urinary catheter insertion
Intraoperative and Postoperative Strategies
- Adherence to sterile technique throughout the procedure
- Minimal use and early removal of urinary catheters
- Prompt wound care and dressing changes
- Early mobilization and hydration to prevent UTI
Complications from Untreated or Delayed E. coli Postoperative Infections
Failure to address E. coli infections promptly may lead to serious complications:
- Pelvic abscess formation
- Urosepsis and septic shock
- Pelvic peritonitis
- Fistula development (e.g., vesicovaginal, rectovaginal)
- Chronic pelvic inflammatory disease
- Prolonged hospitalization and re-operation
- Infertility due to adhesions or tubal damage
Frequently Asked Questions
What is the most common cause of post-op gynecologic infection due to E. coli?
Contamination during surgery or introduction via urinary catheters are primary causes of postoperative E. coli infections.
How soon do symptoms of infection appear after surgery?
Symptoms typically develop within 48 to 96 hours post-surgery but may be delayed in immunocompromised patients.
Is E. coli infection after surgery dangerous?
Yes. If untreated, it can progress to severe complications such as pelvic abscess, peritonitis, or septic shock.
Can postoperative E. coli infections be prevented?
Yes. Preventive measures include sterile surgical techniques, pre-op antibiotic prophylaxis, and proper urinary care.
What is the standard treatment for E. coli in postoperative infections?
Empirical broad-spectrum antibiotics, followed by pathogen-specific therapy based on culture results.
Postoperative gynecological infections due to E. coli are clinically significant complications that require immediate recognition and evidence-based treatment. By integrating microbiological insight with surgical best practices, we can reduce incidence, improve recovery rates, and prevent life-threatening sequelae. Early diagnosis, aggressive antimicrobial therapy, and preventive strategies remain the cornerstone of effective management.