Prevotella species, a group of gram-negative anaerobic bacteria, are increasingly implicated in postoperative gynecologic infections. Commonly found as commensals in the oral cavity, gastrointestinal tract, and female genital tract, they become pathogenic in surgical settings where mucosal barriers are breached. Among them, Prevotella bivia and Prevotella disiens are notably involved in pelvic infections post-gynecologic surgery, often contributing to abscesses, pelvic inflammatory disease, and severe sepsis.
Pathophysiology and Mechanisms of Prevotella Infection
Anaerobic Virulence and Tissue Invasion
Prevotella species thrive in anaerobic conditions, making the postoperative pelvic environment particularly favorable. Their ability to cause disease is attributed to:
- Lipopolysaccharide (LPS): Stimulates inflammatory cytokine production.
- Hydrolytic enzymes (proteases, neuraminidases): Degrade tissue matrix and facilitate invasion.
- Beta-lactamase production: Confers resistance to penicillin-type antibiotics.
- Biofilm formation: Promotes chronic infection and antibiotic resistance.
These factors lead to persistent infections that complicate recovery and often necessitate aggressive medical and surgical intervention.
Risk Factors Contributing to Postoperative Prevotella Infections
Several factors predispose patients to infections by Prevotella following gynecologic procedures:
- Prolonged surgery duration or contamination
- Use of vaginal instrumentation or uterine manipulators
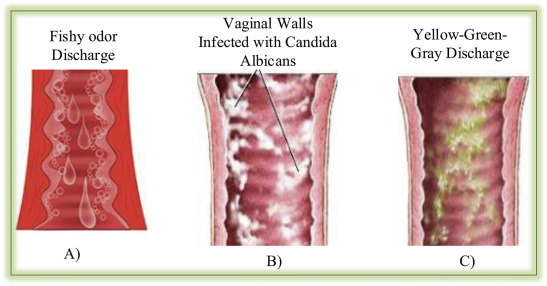
- Pre-existing bacterial vaginosis or sexually transmitted infections
- Immunosuppression, diabetes mellitus, obesity
- Hematoma formation or inadequate drainage
- Inadequate prophylactic antibiotic coverage
Clinical Features and Symptoms of Prevotella-Associated Pelvic Infections
Acute Presentation Post-Surgery
Symptoms usually appear within the first 3–10 days postoperatively. Key signs include:
- Fever > 38.3°C
- Lower abdominal or pelvic pain
- Foul-smelling vaginal discharge
- Localized or diffuse pelvic tenderness
- Signs of wound infection or erythema
- Leukocytosis and elevated inflammatory markers
- Possible signs of septicemia in advanced cases
In advanced infections, tubo-ovarian abscess or peritonitis may develop, requiring emergent management.
Diagnostic Strategies for Detecting Prevotella Infections
Laboratory and Microbiological Investigations
- Complete Blood Count (CBC): Typically shows leukocytosis.
- CRP and ESR: Markedly elevated in systemic involvement.
- Anaerobic culture of aspirated fluid or surgical site: Essential for isolating Prevotella species.
- Gram staining: Reveals small, pleomorphic gram-negative rods.
- PCR and 16S rRNA sequencing: Enhance rapid identification and differentiation of species.
Imaging Techniques
- Transvaginal Ultrasound: Detects pelvic fluid collections or abscesses.
- CT/MRI of pelvis: Offers superior resolution for deep abscesses or retroperitoneal spread.
- Imaging-guided aspiration: Confirms diagnosis and facilitates culture.
Treatment Protocols for Postoperative Prevotella Infections
Antimicrobial Therapy
Initial therapy should cover anaerobic organisms including Prevotella, with adjustments based on culture sensitivity. Common regimens include:
- Empiric Therapy:
- Metronidazole (IV or oral) + third-generation cephalosporin (e.g., ceftriaxone)
- Carbapenems (e.g., ertapenem) in resistant or polymicrobial infections
- Beta-lactam/beta-lactamase inhibitors: Piperacillin-tazobactam is effective
- Duration:
- Uncomplicated cases: 10–14 days
- Complicated cases (abscess/sepsis): 3–4 weeks with close monitoring
Surgical and Interventional Management
- Image-guided percutaneous drainage of pelvic or abdominal abscesses
- Exploratory laparotomy or laparoscopy for uncontrolled infections
- Debridement of infected tissues, removal of necrotic debris or foreign material
Timely intervention minimizes progression to systemic complications.
Prevention of Prevotella Infections Following Gynecologic Surgery
Preoperative Measures
- Screening and treating bacterial vaginosis with metronidazole or clindamycin prior to elective procedures
- Antiseptic vaginal preparation (e.g., povidone-iodine or chlorhexidine)
- Appropriate antibiotic prophylaxis, especially covering anaerobes
Intraoperative Best Practices
- Strict adherence to sterile technique
- Minimizing blood loss and operative time
- Prophylactic drains in patients at high risk of fluid accumulation
Postoperative Monitoring
- Daily wound inspection
- Monitoring of vital signs and inflammatory markers
- Prompt evaluation of any fever or discharge
Complications of Untreated Prevotella Infections
If left unmanaged, Prevotella infections can result in serious outcomes:
- Pelvic abscess or peritonitis
- Tubo-ovarian abscess
- Adhesion formation leading to infertility
- Sepsis and multi-organ failure
- Chronic pelvic pain and dyspareunia
- Need for hysterectomy or oophorectomy in extreme cases
Frequently Asked Questions
What is Prevotella and how does it cause infection?
Prevotella is a gram-negative anaerobic bacterium that causes infection by invading tissue through surgical disruption and releasing inflammatory enzymes.
How is Prevotella infection diagnosed?
Diagnosis involves clinical symptoms, imaging studies, and anaerobic cultures or molecular methods like PCR for accurate identification.
Can Prevotella infections be prevented?
Yes, through proper vaginal antisepsis, antibiotic prophylaxis, and treatment of preexisting genital tract infections before surgery.
Is Prevotella infection life-threatening?
If untreated, it can lead to serious complications including pelvic abscess, sepsis, and even death, especially in immunocompromised patients.
Which antibiotics are effective against Prevotella?
Metronidazole, carbapenems, and beta-lactam/beta-lactamase inhibitor combinations are effective, with therapy adjusted based on resistance profiles.
Postoperative gynecologic infections due to Prevotella demand early identification, targeted antimicrobial therapy, and, when needed, surgical intervention. A multidisciplinary approach combining prevention, diagnostics, and clinical vigilance is essential for successful outcomes. With rising antibiotic resistance and polymicrobial synergy in anaerobic infections, Prevotella species must be considered central agents in any suspected postoperative pelvic infection.

