Postoperative gynecologic infections are significant complications following pelvic surgeries, such as hysterectomies, cesarean sections, and laparoscopic procedures. Anaerobic bacteria, including the Porphyromonas genus—particularly Porphyromonas asaccharolytica and Porphyromonas endodontalis—have emerged as critical pathogens in these infections. These organisms, normally present in mucosal surfaces, become opportunistic pathogens in the altered surgical environment, posing serious risks to patient recovery.
Pathogenesis of Porphyromonas in Gynecologic Infections
Anaerobic Nature and Virulence Mechanisms
Porphyromonas species are gram-negative, obligate anaerobes capable of evading the host immune system and resisting common antimicrobial agents. Key virulence factors include:
- Fimbriae: Facilitate adhesion to epithelial and endothelial cells
- Capsular polysaccharides: Inhibit phagocytosis
- Proteolytic enzymes: Degrade host tissue and immune components
- Hemagglutinins: Promote co-aggregation and biofilm formation
These features enable Porphyromonas to establish persistent infections in anaerobic environments such as pelvic cavities post-surgery.
Risk Factors Predisposing to Porphyromonas-Associated Infections
Several surgical and patient-related factors increase the susceptibility to infections by Porphyromonas species:
- Prolonged operative time
- Contamination with vaginal or rectal flora
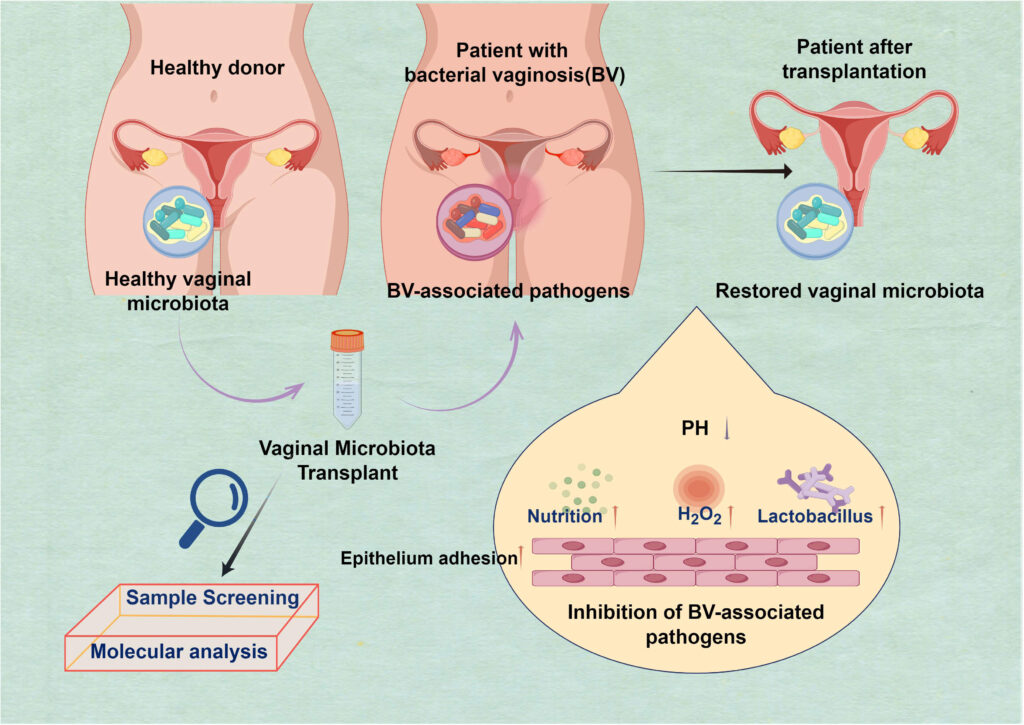
- Pre-existing bacterial vaginosis or PID
- Inadequate sterilization or aseptic technique
- Immunosuppressive conditions (e.g., HIV, chemotherapy)
- Diabetes mellitus
- Poor surgical wound healing or hematoma formation
Clinical Presentation of Postoperative Porphyromonas Infections
Infections typically present within 3 to 7 days post-surgery. Clinical manifestations may include:
- Fever >38.3°C (100.9°F)
- Pelvic pain or cramping
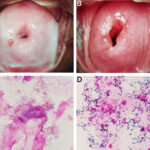
- Foul-smelling or purulent vaginal discharge
- Postoperative wound erythema, tenderness, or discharge
- Localized or diffuse pelvic tenderness
- Delayed return of bowel function
- Sepsis indicators (tachycardia, hypotension, mental status changes)
Diagnostic Approach to Porphyromonas-Induced Pelvic Infections
Laboratory Investigations
- CBC: Leukocytosis with neutrophilic predominance
- C-reactive protein (CRP) and ESR: Marked elevation indicates inflammation
- Blood cultures: May be positive in systemic involvement
Imaging Techniques
- Ultrasound: Useful for identifying pelvic collections or hematomas
- CT scan of abdomen and pelvis: Critical in locating deep abscesses and guiding drainage procedures
Microbiological Identification
- Anaerobic cultures: Must be obtained from wound exudate, aspirated abscess, or surgical site
- MALDI-TOF and PCR: Rapid identification of Porphyromonas species
- Gram stain: Typically shows gram-negative rods with a characteristic morphology
Treatment Strategies for Postoperative Porphyromonas Infections
Empirical and Targeted Antibiotic Therapy
Timely initiation of broad-spectrum antibiotics covering anaerobes is essential:
- First-line empiric regimens:
- Piperacillin-tazobactam
- Ertapenem or meropenem
- Metronidazole + ceftriaxone or ciprofloxacin
- Targeted therapy after culture:
- Adjust based on antibiotic susceptibility
- Porphyromonas often exhibits resistance to clindamycin and macrolides
Duration of treatment generally spans 10 to 14 days, with longer courses for deep or systemic infections.
Surgical and Interventional Management
Drainage and Debridement
- Ultrasound- or CT-guided percutaneous drainage of abscesses
- Surgical re-exploration if peritonitis or widespread infection is present
- Removal of necrotic tissue, infected sutures, or prosthetic material
Supportive Care
- Fluid resuscitation and electrolyte correction
- Antipyretics and pain management
- Monitoring for signs of septic shock
Prevention of Porphyromonas Infections in Gynecologic Surgery
Preoperative Prophylaxis
- Administer prophylactic antibiotics within one hour of incision (e.g., cefazolin with metronidazole)
- Screen and treat bacterial vaginosis or existing vaginal infections pre-surgery
- Adequate bowel preparation when operating near the gastrointestinal tract
Intraoperative Techniques
- Strict asepsis and minimal tissue trauma
- Efficient hemostasis and drainage placement when necessary
- Avoidance of prolonged instrumentation
Postoperative Monitoring and Hygiene
- Early ambulation
- Regular wound inspection
- Glycemic control in diabetic patients
- Prompt response to febrile episodes
Potential Complications of Untreated Infections
If left untreated, Porphyromonas infections can lead to:
- Pelvic abscess
- Pelvic thrombophlebitis
- Sepsis and multi-organ failure
- Adhesion formation and chronic pelvic pain
- Infertility due to fallopian tube damage
- Prolonged hospitalization and reoperation
Prognosis and Follow-Up Care
With early diagnosis and appropriate therapy, outcomes are generally favorable. Follow-up includes:
- Clinical reassessment within 72 hours of initiating antibiotics
- Repeat imaging to confirm resolution of abscesses
- Long-term monitoring for recurrence or residual complications
Frequently Asked Questions
What is Porphyromonas and where is it found?
Porphyromonas is a genus of anaerobic, gram-negative bacteria commonly found in the oral cavity, gastrointestinal tract, and genital tract.
How soon after surgery can Porphyromonas infections appear?
Symptoms typically develop within 3 to 7 days postoperatively, but can emerge earlier in high-risk cases.
Is Porphyromonas resistant to common antibiotics?
Yes, some strains show resistance to macrolides and clindamycin. Sensitivity testing guides effective treatment.
What surgeries pose the highest risk?
Procedures involving the vagina, rectum, or pelvic floor are most susceptible due to proximity to endogenous flora.
Can Porphyromonas infections recur?
Recurrence is possible, particularly in patients with poor immune function or inadequate initial treatment.
Postoperative gynecologic infection due to Porphyromonas represents a growing concern in surgical care. Its anaerobic profile, resistance tendencies, and tissue-destructive capabilities demand prompt diagnosis, aggressive antimicrobial treatment, and, when necessary, surgical intervention. Adherence to preventive protocols and vigilant postoperative surveillance remain essential for reducing morbidity and ensuring favorable outcomes.