Postoperative gynecologic infections are serious complications that can arise after procedures such as hysterectomy, cesarean delivery, myomectomy, or laparoscopic pelvic surgeries. One of the most prevalent anaerobic pathogens implicated in such infections is the genus Bacteroides, particularly Bacteroides fragilis. These bacteria, part of the normal vaginal and intestinal flora, can become pathogenic when translocated into sterile body areas during surgical intervention.
Understanding Bacteroides in Post-Gynecologic Surgery Infections
Anaerobic Pathogenicity of Bacteroides
Bacteroides species are gram-negative, obligate anaerobes that reside in the lower genital tract and intestines. They possess multiple virulence factors:
- Polysaccharide capsule: Resists phagocytosis
- Enzymatic production: Collagenase, hyaluronidase, and heparinase contribute to tissue invasion
- β-lactamase enzymes: Confer resistance to many antibiotics
Once introduced into surgical wounds or pelvic cavities, these bacteria can form abscesses, cause peritonitis, and lead to systemic infections.
Risk Factors for Postoperative Bacteroides Infections
- Prolonged surgery duration
- Contaminated surgical field (e.g., bowel injury)
- Poor aseptic technique
- Diabetes mellitus or immunocompromised state
- Use of foreign bodies (drains, sutures)
- Emergency procedures
- Pre-existing pelvic inflammatory disease (PID)
Clinical Presentation and Symptoms
Post-op gynecologic infections due to Bacteroides typically manifest within 3–10 days after surgery. Key signs include:
- Fever >38°C
- Pelvic or abdominal pain
- Purulent vaginal discharge
- Foul-smelling wound exudate
- Localized pelvic tenderness
- Leukocytosis and elevated CRP
- Wound dehiscence or abscess formation
- Signs of systemic infection or sepsis (tachycardia, hypotension)
Diagnostic Strategies
Laboratory Evaluation
- Complete blood count: Leukocytosis with left shift
- Blood cultures: May isolate anaerobic organisms
- C-reactive protein (CRP) and procalcitonin: Indicators of inflammation
Imaging Techniques
- Transvaginal or abdominal ultrasound: Detects fluid collections or abscesses
- CT scan of the pelvis: Gold standard for visualizing deep-seated infections or post-surgical abscesses
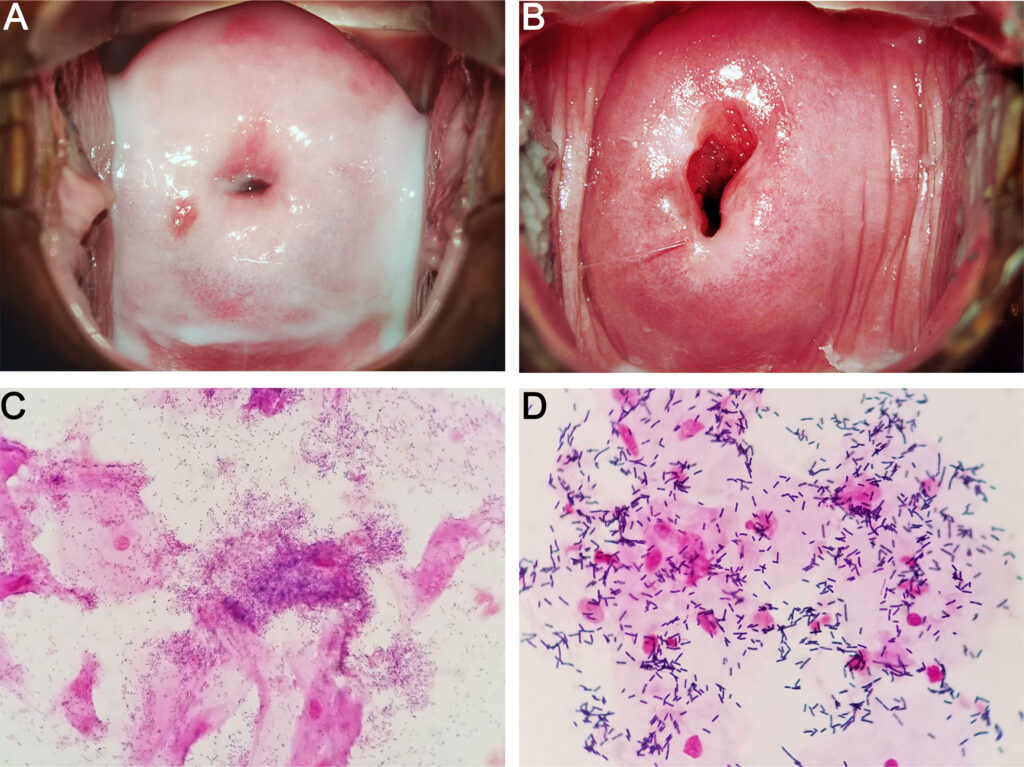
Microbiological Culture
- Anaerobic culture of pus or wound exudate is essential
- Gram stain often shows gram-negative rods
- PCR or MALDI-TOF can aid in rapid identification of Bacteroides fragilis
Treatment Protocols for Bacteroides-Related Infections
Empiric Antibiotic Therapy
Prompt empiric therapy must cover anaerobic organisms:
- First-line options:
- Piperacillin-tazobactam
- Carbapenems (e.g., meropenem, imipenem)
- Metronidazole (effective against anaerobes, often combined with ceftriaxone or ciprofloxacin)
- Alternative regimens:
- Clindamycin (now less favored due to resistance)
- Amoxicillin-clavulanate in mild to moderate infections
Targeted Therapy and Duration
Once culture confirms Bacteroides, adjust therapy based on sensitivities. Treatment duration typically ranges from 7 to 14 days, depending on severity and source control.
Surgical Intervention and Drainage
In cases with abscess formation or extensive pelvic sepsis, surgical drainage becomes essential:
- Image-guided percutaneous drainage (preferred for localized collections)
- Exploratory laparotomy if peritonitis is suspected
- Debridement of infected tissue
- Removal of infected sutures or foreign bodies
Prevention and Prophylaxis
Preoperative Measures
- Bowel prep in indicated surgeries
- Prophylactic antibiotics (e.g., cefazolin + metronidazole) administered within 60 minutes of incision
- Vaginal cleansing with povidone-iodine before surgery
Intraoperative Best Practices
- Minimize tissue handling and surgery duration
- Ensure adequate hemostasis
- Use of sterile techniques and appropriate suture material
- Avoid unnecessary placement of foreign bodies
Postoperative Monitoring
- Early ambulation
- Monitor for signs of infection
- Timely removal of catheters and drains
- Glucose control in diabetic patients
Complications from Untreated Infections
Failure to recognize and manage infections caused by Bacteroides post-surgery can result in:
- Pelvic abscess
- Sepsis and septic shock
- Chronic pelvic pain
- Adhesion formation
- Infertility
- Multiple organ dysfunction syndrome (MODS)
Prognosis and Follow-Up
Early diagnosis, appropriate antibiotic therapy, and surgical intervention (if required) result in favorable outcomes in most patients. Long-term monitoring may be needed in cases involving extensive infections, particularly in immunocompromised individuals.
Frequently Asked Questions
What is the most common Bacteroides species in post-op infections?
Bacteroides fragilis is the most frequently isolated species in post-surgical pelvic infections.
Can Bacteroides infections be life-threatening?
Yes. If untreated, infections can progress to sepsis, which carries high morbidity and mortality.
Is metronidazole sufficient as monotherapy?
Metronidazole is effective against anaerobes but often requires combination therapy to cover gram-negative aerobes and facultative pathogens.
When should imaging be considered?
If fever persists despite antibiotics or if pelvic abscess is suspected, CT or ultrasound imaging is warranted.
Are anaerobic cultures always necessary?
Yes. Identifying the organism guides specific therapy and helps in antibiotic stewardship.
Postoperative gynecologic infections due to Bacteroides present a significant challenge due to the pathogen’s virulence and resistance profile. A multidisciplinary approach involving timely diagnosis, appropriate antimicrobial therapy, and surgical management ensures optimal patient outcomes. Prevention through meticulous surgical practices and prophylaxis remains the most effective strategy to reduce incidence and complications.