Post-menopausal osteoporosis is a progressive bone disease characterized by decreased bone mass and structural deterioration, primarily caused by the sharp decline in estrogen levels following menopause. This condition increases the risk of fractures, especially of the hip, spine, and wrist, significantly impacting morbidity and mortality in older women.
The Role of Estrogen in Bone Integrity
Estrogen plays a crucial role in maintaining bone density by regulating osteoclast activity and reducing bone resorption. After menopause, the ovaries cease estrogen production, accelerating bone loss during the first five to seven years. Women may lose up to 20% of their bone density during this period, underscoring the urgency for early intervention and prevention strategies.
Risk Factors for Post-Menopausal Osteoporosis
Non-Modifiable Risk Factors
- Female sex and age >50
- Early menopause (<45 years)
- Family history of osteoporosis or fragility fractures
- Caucasian or Asian ethnicity
- Low peak bone mass in youth
Modifiable Risk Factors
- Sedentary lifestyle
- Low calcium and vitamin D intake
- Smoking and excessive alcohol use
- Prolonged corticosteroid use
- Inadequate protein intake
Preventive Strategies for Osteoporosis After Menopause
1. Calcium and Vitamin D Intake
Adequate intake of calcium and vitamin D is foundational in maintaining bone health.
- Calcium: Women over 50 should consume 1,200 mg/day through diet and supplements.
- Vitamin D: Recommended intake is 800–1,000 IU/day; optimal serum 25(OH)D level is ≥30 ng/mL.
Sources:
- Calcium: Dairy, leafy greens, fortified foods
- Vitamin D: Sun exposure, fatty fish, fortified milk, supplements
2. Weight-Bearing and Resistance Exercise
Engaging in regular weight-bearing and resistance training exercises helps build and maintain bone mass.
Recommended Activities
- Weight-bearing: Walking, dancing, hiking
- Resistance training: Light weights, resistance bands
- Balance training: Tai chi, yoga to prevent falls
At least 30 minutes, five days a week is advisable, with inclusion of balance and flexibility exercises.
Hormone Replacement and Pharmacologic Therapies
1. Hormone Replacement Therapy (HRT)
HRT is effective in reducing bone resorption and fracture risk when initiated near the onset of menopause.
Indications
- Women with menopausal symptoms and high fracture risk
- Must assess cardiovascular and breast cancer risks prior to initiation
2. Bisphosphonates
First-line pharmacologic treatment for high-risk women.
Common Agents
- Alendronate
- Risedronate
- Ibandronate
- Zoledronic acid
They inhibit osteoclast-mediated bone resorption and are proven to reduce vertebral and hip fractures.
3. Selective Estrogen Receptor Modulators (SERMs)
Raloxifene mimics estrogen’s effects on bones without affecting the uterus or breast. It’s particularly beneficial for vertebral fracture prevention.
4. Denosumab
A monoclonal antibody that inhibits RANKL and reduces osteoclast formation, prescribed for post-menopausal women at high fracture risk or intolerant to bisphosphonates.
5. Anabolic Therapies
Agents like teriparatide and abaloparatide stimulate bone formation and are reserved for severe osteoporosis or multiple fractures.
Screening and Diagnosis
Bone Mineral Density (BMD) Testing
Dual-energy X-ray Absorptiometry (DEXA) is the gold standard for measuring BMD.
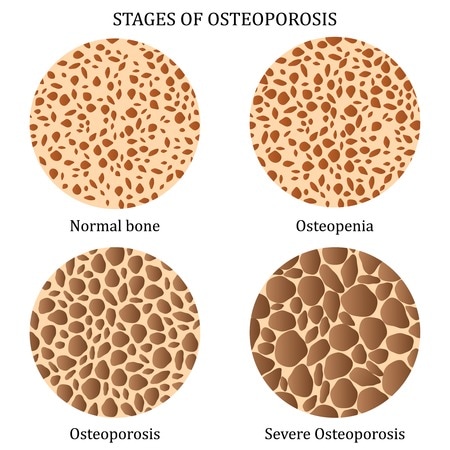
Interpretation
- T-score ≥ -1.0: Normal
- T-score between -1.0 and -2.5: Osteopenia
- T-score ≤ -2.5: Osteoporosis
Screening is recommended:
- At age 65 and older
- Or younger post-menopausal women with risk factors
FRAX Tool
Estimates the 10-year probability of a major osteoporotic fracture and guides treatment decisions.
Nutrition Beyond Calcium and Vitamin D
Protein
Adequate protein intake supports bone matrix and muscle strength.
Magnesium, Vitamin K2, and Zinc
These nutrients support bone mineralization and remodeling.
Phytoestrogens
Found in soy, flaxseed, and legumes, phytoestrogens may provide mild estrogen-like effects beneficial for bone health.
Lifestyle Modifications for Long-Term Bone Protection
Smoking Cessation and Alcohol Reduction
Tobacco and excessive alcohol interfere with calcium absorption and bone metabolism.
Fall Prevention
Install home safety features, correct vision issues, and wear proper footwear to reduce fracture risk.
Sunlight Exposure
Encourages natural vitamin D synthesis. A 10–15 minute daily exposure without sunscreen is generally sufficient.
FAQs:
What is the most effective treatment for osteoporosis after menopause?
Bisphosphonates and denosumab are most effective for fracture prevention, especially when combined with lifestyle changes and adequate nutrition.
Can osteoporosis be reversed after menopause?
While it cannot be fully reversed, bone loss can be slowed and partially rebuilt with medications like teriparatide and proper lifestyle interventions.
When should I start screening for osteoporosis?
Women should begin screening at age 65, or earlier if other risk factors are present.
How long should I take osteoporosis medication?
Treatment duration varies; bisphosphonates may be paused after 3–5 years in low-risk individuals. Continuous reassessment is essential.
Is hormone therapy safe for osteoporosis prevention?
HRT is effective but not suitable for everyone due to cardiovascular and cancer risks. It must be individualized.
Prevention of post-menopausal osteoporosis is a critical aspect of women’s health that demands early intervention, informed lifestyle choices, and when appropriate, pharmacologic therapy. Through comprehensive strategies encompassing nutrition, physical activity, screening, and clinical treatment, we can significantly reduce the burden of fractures and preserve quality of life in post-menopausal women. The combined efforts of patients, clinicians, and public health systems are essential to curb the silent progression of osteoporosis.