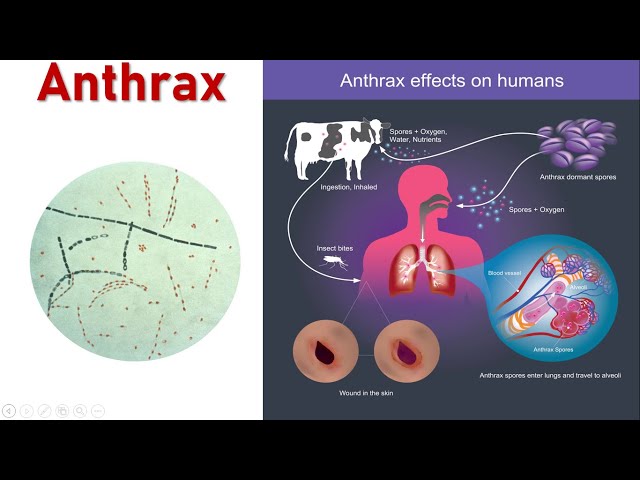
Anthrax is a serious zoonotic disease caused by Bacillus anthracis, a spore-forming, Gram-positive bacterium. Human infection typically occurs through contact with infected animals or their by-products or through deliberate biological exposure. The inhalational form is the most lethal, and post-exposure prevention measures are critical to reduce mortality following suspected or confirmed exposure.
Transmission and Types of Anthrax
Routes of Anthrax Infection
- Inhalation – Most fatal, due to aerosolized spores
- Cutaneous – Most common, through skin abrasions
- Gastrointestinal – Rare, through ingestion of contaminated meat
- Injection – Linked to illicit drug use in some regions
Why Inhalation Exposure Demands Immediate Action
Inhaled spores can remain dormant in the lungs for weeks. Without treatment, once germination begins, toxins lead to rapid systemic infection, often resulting in septic shock and death.
Post-Exposure Prophylaxis (PEP) for Anthrax
1. Antibiotic Therapy
Immediate administration of antibiotics is the cornerstone of post-exposure anthrax prevention.
Recommended First-Line Antibiotics
- Ciprofloxacin (500 mg orally twice daily)
- Doxycycline (100 mg orally twice daily)
Alternative Options
- Levofloxacin, Amoxicillin (if B. anthracis is known to be penicillin-sensitive and patient is not allergic)
Duration
- 60 days of antibiotic treatment is required due to the prolonged incubation period of inhaled anthrax spores.
2. Anthrax Vaccine Adsorbed (AVA)
Also known as BioThrax®, the anthrax vaccine is administered concurrently with antibiotics to enhance protection.
PEP Vaccination Schedule
- 3-dose series: Day 0, Day 14, Day 28
- Administered intramuscularly
- Only authorized under emergency use or specific public health scenarios
Clinical Symptoms to Monitor Post-Exposure
Inhalation Anthrax Symptoms
- Initial flu-like symptoms (fever, fatigue, cough)
- Rapid progression to severe respiratory distress
- Cyanosis, diaphoresis, shock
- Mediastinal widening on chest X-ray
- High mortality rate without early intervention
Cutaneous Anthrax Symptoms
- Painless ulcer with black eschar
- Swelling and redness around the site
- Low mortality with treatment
Gastrointestinal Symptoms
- Severe abdominal pain
- Nausea, vomiting, bloody diarrhea
- Sepsis may occur in advanced stages
Laboratory Testing and Diagnosis
Diagnostic Tools
- Polymerase Chain Reaction (PCR) – Detects B. anthracis DNA
- Blood cultures – Especially in systemic cases
- Chest imaging – Reveals mediastinal widening in inhalation anthrax
- Immunohistochemistry (IHC) – Identifies anthrax antigens in tissue
Early diagnosis significantly improves survival outcomes in inhalation anthrax cases.
Emergency Public Health Protocols
1. Exposure Assessment
- Immediate environmental testing at suspected contamination sites
- Epidemiologic investigation to identify exposed individuals
- Coordination with CDC and local health departments
2. Mass Prophylaxis
- Dispensing of antibiotics and vaccine via Points of Dispensing (PODs)
- Education on adherence to 60-day antibiotic regimen
- Use of Strategic National Stockpile (SNS) for medical supplies
3. Decontamination Procedures
- Personal decontamination with soap and water
- Facility decontamination with EPA-approved sporicidal agents
- Air handling and surface testing post-cleanup
Special Populations and Considerations
Pregnant or Lactating Women
- Ciprofloxacin is preferred; AVA vaccine can be administered if benefits outweigh risks.
Children
- Pediatric dosages adjusted by weight; ciprofloxacin and doxycycline are safe under CDC guidance.
Immunocompromised Individuals
- Require close clinical monitoring; vaccination should still be administered as part of PEP.
Long-Term Monitoring and Psychological Impact
Surveillance Post-PEP
- Monitor for delayed symptom onset even after prophylaxis
- Report adverse events from vaccine or antibiotics to VAERS
Psychosocial Support
- Address anxiety and PTSD resulting from bioterrorism-related exposure
- Provide counseling and community outreach services
Frequently Asked Questions:
What should I do if I suspect anthrax exposure?
Seek immediate medical attention. Do not wait for symptoms. Begin antibiotics as directed and follow public health instructions.
Is the anthrax vaccine available to the general public?
No. It is reserved for military personnel, lab workers, and those exposed in confirmed anthrax incidents.
Can anthrax be transmitted from person to person?
No. Anthrax is not contagious through human contact. Infection occurs via spores from the environment.
Why is a 60-day antibiotic course required?
Anthrax spores can remain dormant in the body for weeks. A 60-day course ensures eradication as they germinate.
What happens if I miss a vaccine dose?
Contact your healthcare provider immediately to reschedule. Maintaining the timeline is crucial for full protection.
Effective post-exposure anthrax prevention hinges on rapid response, strict adherence to a 60-day antibiotic regimen, and timely administration of the anthrax vaccine. Inhalation anthrax, while rare, remains a serious bioterrorism threat with high fatality rates if untreated. Coordinated public health action, patient compliance, and community preparedness are vital components in preventing widespread illness following exposure.