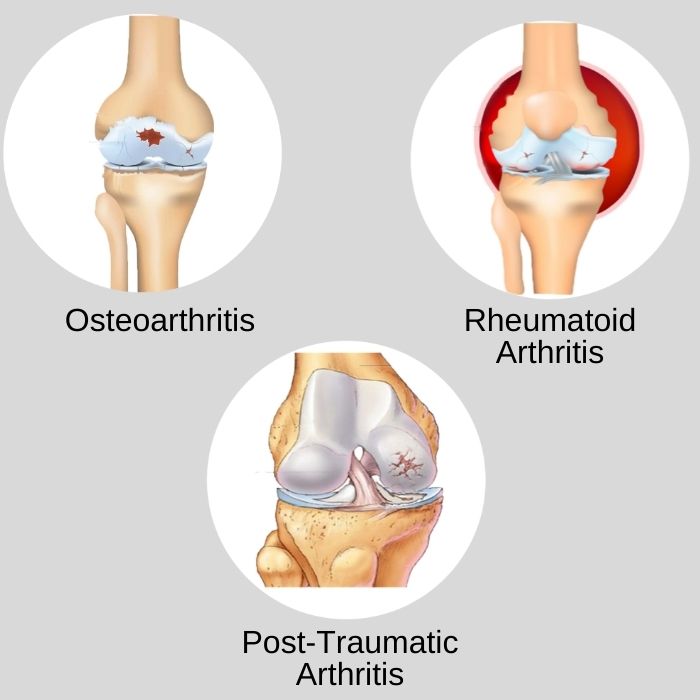
Post-traumatic osteoarthritis (PTOA) is a chronic, degenerative joint condition that develops following a traumatic injury to a joint. Unlike primary osteoarthritis, which typically arises from age-related wear and tear, PTOA results directly from physical damage, such as fractures, ligament tears, or cartilage injuries. It most commonly affects weight-bearing joints like the knee, ankle, hip, and shoulder, and can significantly impair function and quality of life.
Pathophysiology of Post-Traumatic Osteoarthritis
Trauma to a joint initiates a cascade of mechanical and biochemical changes that accelerate cartilage degradation. The impact of trauma causes inflammation, chondrocyte death, and matrix breakdown, leading to joint space narrowing, osteophyte formation, and bone remodeling. Over time, the cartilage loses its ability to cushion the joint, resulting in pain and stiffness.
Common Causes and Risk Factors
PTOA can result from a variety of acute and repetitive injuries that compromise joint stability and cartilage integrity.
Major Causes:
- Intra-articular fractures (e.g., tibial plateau, distal femur)
- Anterior cruciate ligament (ACL) tears
- Meniscus injuries
- Dislocations of the shoulder, hip, or knee
- Repetitive joint overuse in athletes or laborers
Risk Factors:
- Severity of initial trauma
- Inadequate treatment or rehabilitation
- Obesity
- Joint malalignment
- Genetic predisposition
Symptoms of Post-Traumatic Osteoarthritis
The symptoms of PTOA can appear months to years after the initial injury and may progress gradually. They are similar to those of primary osteoarthritis but often occur at a younger age.
Common Symptoms:
- Persistent joint pain, worsened by activity
- Swelling and inflammation
- Joint stiffness, especially after rest
- Reduced range of motion
- Creaking or grinding sounds (crepitus)
- Instability or joint locking
Diagnosis and Clinical Evaluation
Accurate diagnosis of PTOA relies on a combination of clinical history, physical examination, and imaging studies.
Diagnostic Steps:
1. Medical History
- Previous joint injuries, surgeries, or instability
- Onset and progression of symptoms
2. Physical Examination
- Tenderness along the joint line
- Crepitus with movement
- Joint laxity or deformity
3. Imaging Modalities
- X-rays: Joint space narrowing, osteophyte formation, subchondral sclerosis
- MRI: Assessment of cartilage, menisci, ligaments, and synovial inflammation
- CT scans: For complex intra-articular fractures or surgical planning
Treatment Options for Post-Traumatic Osteoarthritis
The management of PTOA is tailored to the severity of symptoms, extent of joint damage, and functional impairment. Both non-surgical and surgical options are employed.
Non-Surgical Management
1. Pharmacologic Therapy
- NSAIDs (e.g., ibuprofen, naproxen) to reduce pain and inflammation
- Topical analgesics
- Corticosteroid injections for temporary relief
- Hyaluronic acid injections to improve lubrication
2. Physical Therapy
- Strengthening exercises to support joint stability
- Range of motion and flexibility training
- Low-impact aerobic conditioning (e.g., swimming, cycling)
3. Lifestyle Modifications
- Weight management to reduce joint stress
- Activity modification to avoid repetitive strain
- Use of braces, canes, or orthotic supports
Surgical Management
Surgery is considered when conservative measures fail and quality of life is significantly compromised.
Common Surgical Interventions:
- Arthroscopy: For debridement or removal of loose fragments
- Osteotomy: Realignment procedures to redistribute joint forces
- Joint fusion (arthrodesis): For severe pain in smaller joints
- Total joint arthroplasty (replacement): For end-stage PTOA, especially in knees or hips
Preventive Strategies for High-Risk Individuals
Early intervention following joint trauma is critical in preventing or delaying the onset of PTOA.
Key Preventive Measures:
- Prompt and appropriate treatment of joint injuries
- Anatomic fracture reduction and stabilization
- Structured rehabilitation programs
- Correction of joint malalignment
- Use of protective equipment during sports or occupational activities
Prognosis and Long-Term Outlook
The prognosis for PTOA varies depending on the nature of the injury, timing of treatment, and adherence to rehabilitation. While PTOA is progressive and irreversible, early diagnosis and multidisciplinary management can significantly alleviate symptoms and delay joint deterioration.
Many patients with PTOA maintain an active lifestyle with conservative care, while others may require surgical intervention to restore joint function and improve quality of life.
Post-traumatic osteoarthritis represents a complex interplay of mechanical damage, inflammatory processes, and biological degeneration following joint injury. Through a combination of early diagnosis, individualized treatment, and preventive strategies, we can effectively manage this condition and help patients regain optimal joint health and function.