Polymyositis is a chronic inflammatory myopathy that primarily targets skeletal muscles, leading to progressive muscle weakness. As an autoimmune disorder, it arises when the immune system mistakenly attacks muscle fibers, particularly those closest to the trunk such as the shoulders, hips, neck, and thighs. It belongs to a group of disorders known as idiopathic inflammatory myopathies (IIMs) and may coexist with other autoimmune diseases or systemic conditions.
Polymyositis is more commonly diagnosed in adults between the ages of 30 and 60 and has a higher prevalence in females. Although rare, it is a serious and debilitating condition that requires a timely, multidisciplinary approach to treatment and management.
Pathophysiology of Polymyositis
Polymyositis is characterized by T-cell mediated cytotoxicity directed against muscle fibers. The pathology involves:
- Infiltration of CD8+ cytotoxic T-cells
- Overexpression of MHC Class I molecules on muscle cells
- Destruction of muscle fibers by immune cells
- Degeneration and regeneration cycles in muscle tissue
This immune-driven muscle inflammation leads to muscle fiber necrosis, atrophy, and fibrosis over time, resulting in progressive muscle dysfunction.
Causes and Risk Factors
The exact etiology of polymyositis remains unknown, but it is believed to result from a complex interplay of genetic, immunologic, and environmental factors.
Potential Triggers:
- Viral infections (e.g., HIV, HTLV-1, Coxsackievirus)
- Certain medications (e.g., statins, penicillamine)
- Malignancies (paraneoplastic syndrome)
- Autoimmune overlap syndromes
Risk Factors:
- Age 30–60
- Female sex
- Personal or family history of autoimmune disease
- Coexisting connective tissue disorders (e.g., SLE, scleroderma)
Key Symptoms of Polymyositis
The hallmark of polymyositis is symmetrical proximal muscle weakness that develops gradually over weeks to months. Unlike dermatomyositis, skin involvement is absent.
Common Symptoms:
- Progressive weakness in shoulders, hips, neck, and thighs
- Difficulty rising from a chair, climbing stairs, lifting objects
- Fatigue and muscle discomfort
- Dysphagia (difficulty swallowing) in advanced stages
- Shortness of breath due to diaphragmatic involvement
Systemic Symptoms:
- Low-grade fever
- Weight loss
- Arthralgia (joint pain)
- Raynaud’s phenomenon (in some overlap syndromes)
Diagnostic Criteria and Investigations
Diagnosis of polymyositis is based on clinical features, laboratory evidence, electromyographic (EMG) findings, and muscle biopsy.
Laboratory Findings:
- Elevated muscle enzymes:
- Creatine kinase (CK)
- Aldolase
- Lactate dehydrogenase (LDH)
- Elevated ESR and CRP
- Positive autoantibodies:
- Anti-Jo-1 (most common)
- ANA (antinuclear antibody)
Imaging and Electrophysiology:
- MRI: Muscle inflammation and edema
- EMG: Myopathic changes and spontaneous fibrillations
- Muscle Biopsy:
- Endomysial inflammation
- CD8+ T-cell infiltration
- Fiber necrosis and regeneration
Differential Diagnoses:
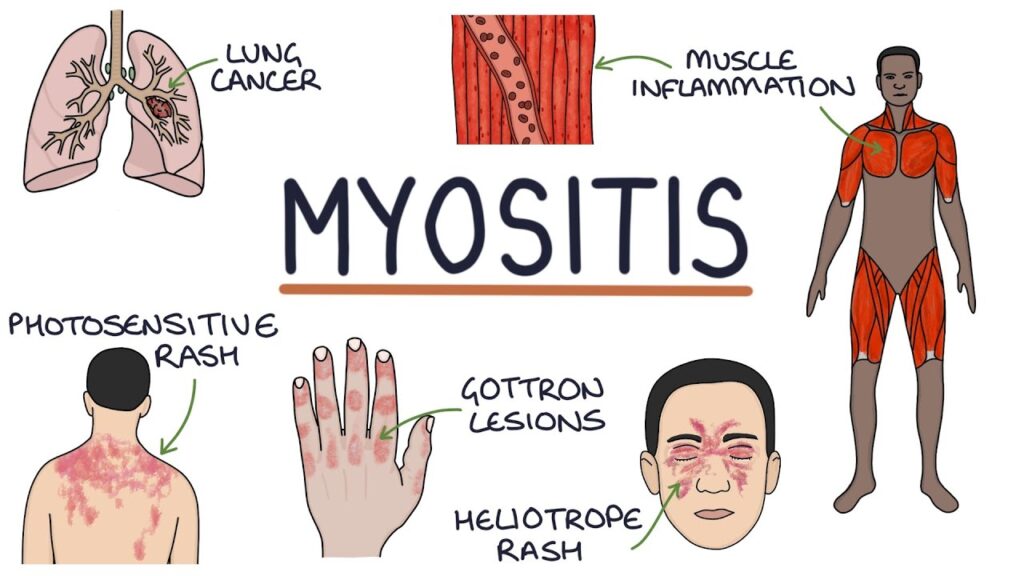
- Dermatomyositis
- Inclusion body myositis
- Muscular dystrophy
- Hypothyroid myopathy
- Drug-induced myopathy
Polymyositis and Associated Conditions
Polymyositis is often associated with other systemic or autoimmune diseases. Careful evaluation for overlap syndromes and malignancies is essential.
Common Associations:
- Interstitial lung disease (ILD)
- Systemic sclerosis
- Rheumatoid arthritis
- Malignancies (especially in older adults)
Cancer Screening:
- Recommended in all new PM patients over age 50
- Age-appropriate screening (mammogram, colonoscopy, CT chest/abdomen/pelvis)
Treatment Options for Polymyositis
1. Corticosteroids
- First-line therapy
- Prednisone 1 mg/kg/day
- Taper after 4–6 weeks once clinical response achieved
2. Immunosuppressive Agents
- Used in steroid-resistant or relapsing cases
- Methotrexate or Azathioprine (commonly used)
- Mycophenolate mofetil or Tacrolimus (in refractory cases)
3. Biologic Therapies
- Rituximab or IVIG for resistant cases
- Targeted immunomodulation in severe or life-threatening disease
4. Supportive Therapy
- Physical therapy: Essential to prevent atrophy and restore strength
- Speech therapy: For dysphagia
- Nutritional support: In cases of muscle wasting or dysphagia
Monitoring and Long-Term Management
Polymyositis requires ongoing monitoring and adjustment of therapy based on disease activity and side effects.
Monitoring Parameters:
- Muscle enzyme levels (CK, Aldolase)
- Pulmonary function tests (if ILD suspected)
- Periodic imaging to assess muscle status
- Regular assessment for medication toxicity
Relapse Indicators:
- Return of muscle weakness
- Rise in CK or inflammatory markers
- Worsening of associated organ involvement
Prognosis and Complications
With early diagnosis and appropriate therapy, most patients respond well to treatment. However, relapses are common and may require long-term immunosuppression.
Prognostic Factors:
- Better: Early diagnosis, good steroid response, no malignancy
- Worse: Presence of ILD, malignancy, delayed treatment
Possible Complications:
- Respiratory failure from muscle weakness
- Dysphagia-related aspiration pneumonia
- Osteoporosis from long-term steroid use
- Muscle atrophy from inactivity
Polymyositis is a rare but potentially debilitating autoimmune myopathy that necessitates early recognition, aggressive treatment, and multidisciplinary care. With the right combination of pharmacologic and supportive therapies, patients can achieve remission and maintain a high quality of life. Continuous monitoring and a personalized treatment approach remain critical in managing this complex condition effectively.