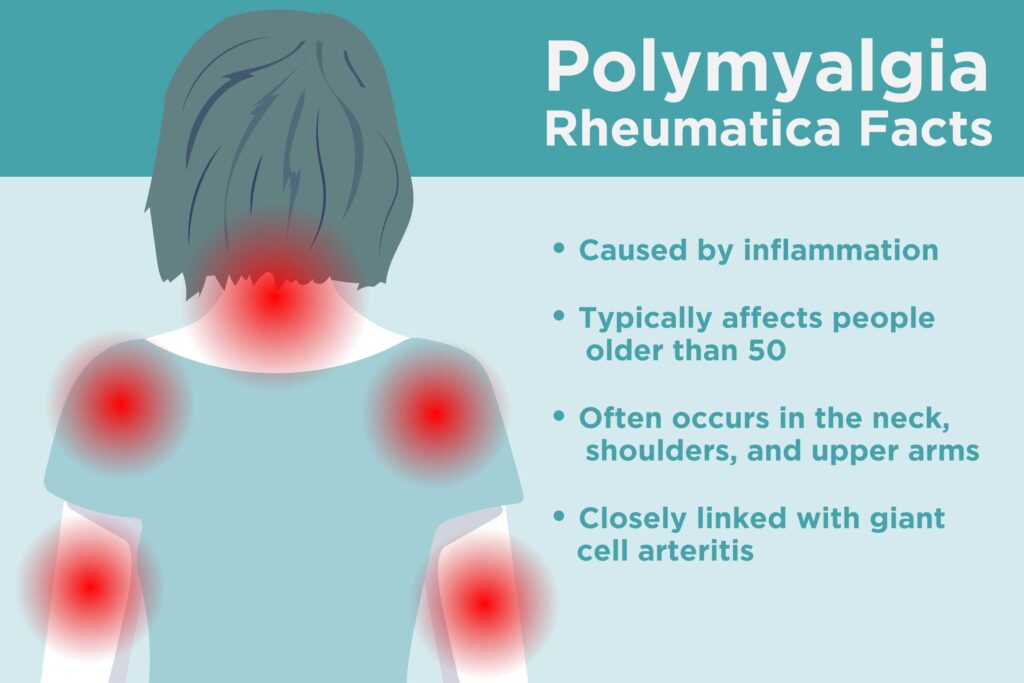
Polymyalgia rheumatica (PMR) is a chronic inflammatory disorder predominantly affecting adults over the age of 50. Characterized by pain and stiffness in the shoulders, neck, and hips, PMR is an immune-mediated condition that typically arises suddenly and symmetrically. It is closely associated with giant cell arteritis (GCA), a form of vasculitis, with up to 20% of PMR patients developing GCA.
PMR is not a form of arthritis but rather a systemic rheumatic condition primarily involving the muscles and soft tissues. While the exact cause remains unknown, it is widely believed to result from a combination of genetic susceptibility and environmental triggers that initiate an autoimmune response.
Causes and Risk Factors of Polymyalgia Rheumatica
The etiology of PMR remains uncertain, but several contributing factors have been identified through epidemiological and immunological research.
Potential Causes:
- Immune system dysfunction: Abnormal immune responses may lead to chronic inflammation.
- Genetic predisposition: HLA-DR4 and HLA-DRB1 alleles have been implicated.
- Infectious triggers: Viral infections (e.g., parvovirus B19, adenovirus) are hypothesized to initiate immune activation in predisposed individuals.
Risk Factors:
- Age >50 years (peak incidence at 70–80 years)
- Female sex (2–3 times more common in women)
- Northern European descent
- Family history of autoimmune diseases
Key Symptoms of Polymyalgia Rheumatica
PMR presents with a distinct clinical profile that often allows for a prompt diagnosis. The hallmark symptom is bilateral muscle pain and stiffness, particularly in the shoulders and hips, which is worse in the morning and improves with movement.
Primary Symptoms:
- Sudden onset of proximal muscle pain and stiffness
- Morning stiffness lasting more than 45 minutes
- Restricted range of motion
- Low-grade fever, fatigue, and weight loss
- Depression or malaise due to persistent inflammation
Associated Conditions:
- Giant Cell Arteritis (GCA): Headache, scalp tenderness, visual disturbances, and jaw claudication. Early identification is critical due to risk of permanent vision loss.
Diagnosis of Polymyalgia Rheumatica
PMR is primarily diagnosed clinically, supported by laboratory findings and the exclusion of other differential diagnoses.
Diagnostic Criteria:
- Age ≥50 years
- Bilateral shoulder aching
- Elevated erythrocyte sedimentation rate (ESR) and/or C-reactive protein (CRP)
- Rapid and dramatic response to low-dose corticosteroids
- Symptoms present for at least two weeks
Supportive Investigations:
- ESR >40 mm/hr and/or CRP >10 mg/L
- Anemia of chronic disease
- Ultrasound: Bursitis or synovitis in shoulders and hips
- PET scan: May detect subclinical GCA
Differential Diagnoses:
- Rheumatoid arthritis
- Myositis
- Hypothyroidism
- Fibromyalgia
- Malignancies
Treatment Strategies for Polymyalgia Rheumatica
The cornerstone of PMR treatment is glucocorticoid therapy, which typically produces a dramatic improvement within days.
1. Glucocorticoids (First-line Treatment)
- Initial dose: 10–20 mg/day of prednisone
- Taper gradually over 12–18 months
- Monitor for relapse: return of stiffness or elevated inflammatory markers
2. Steroid-Sparing Agents
- Considered for patients requiring long-term steroids or with frequent relapses
- Methotrexate: Most commonly used adjunct
- Tocilizumab: IL-6 receptor blocker, beneficial in steroid-resistant cases
3. Management of Side Effects
- Calcium and vitamin D supplementation
- Bisphosphonates to prevent osteoporosis
- Regular blood pressure and glucose monitoring
- Lifestyle modifications: Exercise, diet, smoking cessation
Monitoring and Long-Term Management
Effective long-term management of PMR includes monitoring inflammatory markers, assessing response to therapy, and ensuring patient education to recognize signs of relapse or GCA.
Follow-Up Protocol:
- Regular ESR/CRP checks
- Monitor for steroid-related side effects
- Adjust tapering schedule based on symptoms and labs
- Annual bone density scan for patients on long-term steroids
Relapse Indicators:
- Return of proximal stiffness or pain
- Re-elevation of CRP/ESR after dose reduction
- Systemic symptoms (e.g., fatigue, malaise)
Prognosis and Outlook for Patients with PMR
With appropriate treatment, most individuals with PMR achieve remission and resume normal daily activities. The median duration of treatment is between 1 to 2 years, although some may require a longer course.
Prognostic Factors:
- Favorable: Prompt response to steroids, absence of GCA
- Unfavorable: Steroid dependency, relapsing disease, GCA involvement
Note: PMR does not cause permanent muscle damage but can impact quality of life without proper management.
Polymyalgia rheumatica is a highly treatable inflammatory condition with a distinct clinical pattern that allows for early recognition and intervention. Prompt initiation of corticosteroids yields rapid symptom relief, and comprehensive care ensures optimal long-term outcomes. Close monitoring, patient education, and awareness of potential complications like giant cell arteritis remain vital in achieving disease control and preventing irreversible consequences.