Bacteroides tubo-ovarian abscess represent a severe form of pelvic inflammatory disease (PID), often involving complex infections that affect the fallopian tubes and ovaries. Among the various causative pathogens, Bacteroides species play a critical role. These anaerobic bacteria are part of the normal flora in the gastrointestinal and genital tracts but can become pathogenic under specific conditions, leading to severe complications.
What Is a Tubo-Ovarian Abscess?
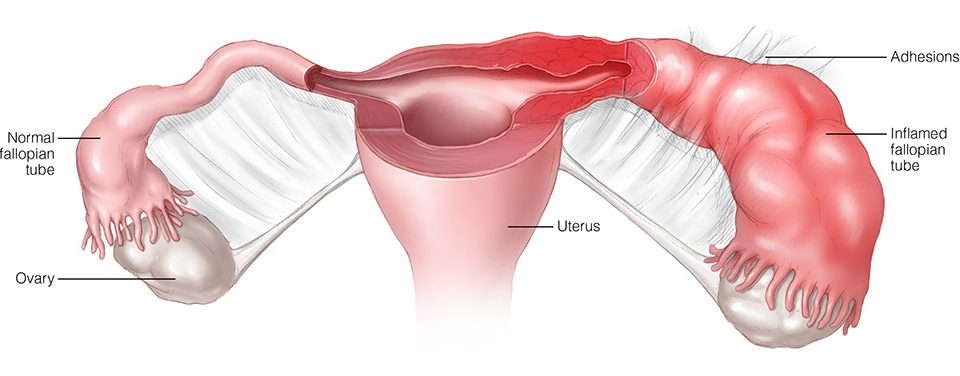
A tubo-ovarian abscess is a localized collection of pus involving the fallopian tubes, ovaries, or adjacent pelvic structures. It frequently arises as a complication of untreated or inadequately treated PID. TOAs are typically polymicrobial, involving aerobic and anaerobic bacteria, with Bacteroides species being a significant contributor.
Pathophysiology of TOAs
TOAs develop when ascending infections spread from the lower genital tract to the upper reproductive organs. The following processes contribute to their formation:
- Disruption of epithelial barriers.
- Inflammatory response to infection.
- Localized pus accumulation.
Role of Bacteroides in Tubo-Ovarian Abscess
Bacteroides species, particularly Bacteroides fragilis, are anaerobic gram-negative bacteria. Although they normally exist symbiotically within the human body, they can act as opportunistic pathogens under certain conditions. Their role in TOAs stems from their ability to:
- Produce virulence factors, such as capsular polysaccharides, that evade the host immune response.
- Generate enzymes that degrade host tissues and facilitate abscess formation.
- Resist antibiotics through mechanisms like beta-lactamase production.
Clinical Presentation
Symptoms
Patients with TOAs often present with nonspecific yet severe symptoms, including:
- Acute or chronic pelvic pain.
- Fever and chills.
- Vaginal discharge, often purulent.
- Dyspareunia (pain during intercourse).
- Abnormal uterine bleeding.
Risk Factors
- History of pelvic inflammatory disease.
- Intrauterine device (IUD) usage.
- Recent gynecological procedures.
- Multiple sexual partners.
- Immunosuppressive conditions.
Diagnosis
Accurate and prompt diagnosis of TOAs is critical to prevent severe complications like sepsis or infertility.
Clinical Evaluation
- History and Physical Examination:
- Tenderness in the adnexal regions.
- Cervical motion tenderness.
- Imaging Studies:
- Ultrasound: First-line imaging for detecting abscesses.
- CT Scan: Useful for complex cases or differential diagnosis.
- MRI: Provides detailed imaging in ambiguous cases.
Laboratory Tests
- Elevated inflammatory markers, such as C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR).
- Leukocytosis on complete blood count (CBC).
- Microbial cultures from aspirated abscess fluid to confirm Bacteroides involvement.
Treatment
Management of TOAs requires a combination of medical and, in some cases, surgical approaches.
Antibiotic Therapy
Broad-spectrum antibiotics effective against both aerobic and anaerobic bacteria are the cornerstone of treatment. Common regimens include:
- Metronidazole combined with cephalosporins or fluoroquinolones.
- Clindamycin for severe cases involving resistant Bacteroides strains.
Surgical Intervention
Surgical management is indicated in cases of:
- Large abscesses (>7 cm).
- Ruptured abscesses causing peritonitis.
- Lack of response to antibiotic therapy.
Procedures include:
- Ultrasound-guided aspiration.
- Laparoscopic drainage.
- Salpingo-oophorectomy in extreme cases.
Prevention
Preventive strategies focus on mitigating risk factors for PID and subsequent TOA development:
- Regular gynecological check-ups.
- Prompt treatment of sexually transmitted infections.
- Proper IUD insertion and monitoring.
- Safe sexual practices, including condom use.
MYHEALTHMAG