Polyarticular juvenile idiopathic arthritis (JIA) is a chronic autoimmune condition affecting five or more joints during the first six months of disease onset in children under 16 years. This subtype of JIA resembles adult rheumatoid arthritis and is characterized by persistent joint inflammation, stiffness, and pain, potentially leading to joint damage if untreated.
There are two main forms of polyarticular JIA:
- Rheumatoid factor (RF)-positive, which closely mimics adult rheumatoid arthritis.
- RF-negative, which typically has a milder course.
Causes and Risk Factors
The precise cause of polyarticular JIA remains unknown, but it is believed to arise from a combination of genetic predisposition and environmental triggers that misdirect the immune system to attack joint tissues.
Key risk factors include:
- Family history of autoimmune diseases
- Female gender (more common in girls)
- Presence of certain HLA (human leukocyte antigen) genes
- Exposure to viral or bacterial infections that may trigger immune dysregulation
Clinical Presentation and Symptoms
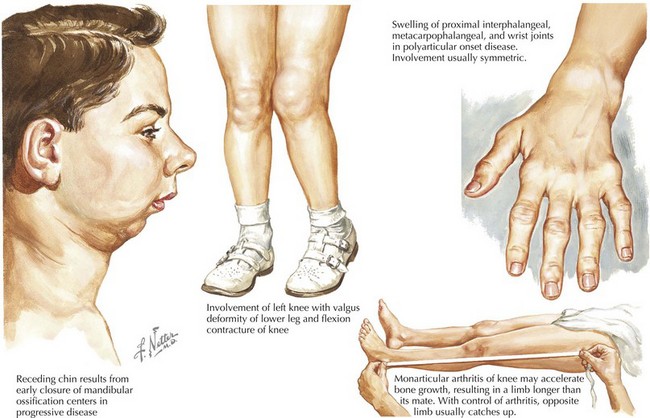
Children with polyarticular JIA often present with symmetrical joint involvement affecting small joints (e.g., hands and feet), but larger joints such as knees and wrists can also be involved.
Common symptoms include:
- Persistent joint pain and swelling
- Morning stiffness lasting more than 30 minutes
- Fatigue and low-grade fevers
- Decreased physical activity or limping
- Weight loss in more severe cases
In RF-positive cases, the disease tends to be more aggressive and is often associated with erosive joint damage.
Diagnostic Evaluation
Early diagnosis is crucial for effective management and prevention of long-term joint destruction.
Diagnostic Criteria:
- Arthritis in five or more joints within the first six months
- Age of onset before 16 years
- Symptoms lasting more than six weeks
Laboratory Tests:
- Rheumatoid factor (RF): Positive in a subset of cases
- Anti-cyclic citrullinated peptide (anti-CCP) antibodies: Indicative of more severe disease
- Erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP): Elevated in active inflammation
- ANA (antinuclear antibodies): May be positive, especially in RF-negative patients
Imaging:
- X-rays: Assess joint space narrowing and erosion
- Ultrasound or MRI: Detect early synovitis and monitor disease progression
Treatment Options for Polyarticular JIA
1. Nonsteroidal Anti-inflammatory Drugs (NSAIDs)
First-line therapy for pain and inflammation reduction. Common agents include naproxen and ibuprofen.
2. Disease-Modifying Antirheumatic Drugs (DMARDs)
Methotrexate remains the gold standard for moderate to severe disease and may be combined with biologics in refractory cases.
3. Biologic Therapies
Targeted therapies for patients who do not respond adequately to DMARDs:
- TNF inhibitors: Etanercept, adalimumab
- IL-6 receptor antagonists: Tocilizumab
- CTLA-4-Ig: Abatacept
4. Corticosteroids
Used for severe flare-ups or systemic involvement. Oral or intra-articular administration depending on severity.
5. Physical and Occupational Therapy
Essential to maintain joint function, muscle strength, and prevent contractures.
Prognosis and Long-term Management
The course of polyarticular JIA varies. RF-positive patients often experience a more persistent and severe disease with risk of permanent joint damage. Early initiation of aggressive treatment can improve outcomes significantly.
Ongoing management includes:
- Regular monitoring of disease activity
- Adjustments in medication regimen
- Screening for side effects of long-term therapy
- Psychological support for chronic illness adaptation
Complications Associated with Polyarticular JIA
Without timely and effective treatment, patients may develop:
- Joint deformities and growth disturbances
- Osteopenia or osteoporosis due to chronic inflammation or corticosteroid use
- Uveitis, particularly in ANA-positive patients
- Functional disability and reduced quality of life
Living with Polyarticular JIA: Family and School Considerations
Support systems are vital in helping children cope with JIA. Collaboration between families, healthcare providers, and educational institutions ensures that children receive necessary accommodations and emotional support.
Recommended strategies:
- Individualized Education Plans (IEPs)
- Flexibility in physical activities
- Counseling and peer support groups
Preventive Measures and Monitoring
Although polyarticular JIA cannot be prevented, early recognition and continuous disease monitoring are crucial.
Regular assessments should include:
- Growth measurements
- Eye exams to detect asymptomatic uveitis
- Bone density evaluations
- Lab work for treatment toxicity surveillance
Polyarticular juvenile idiopathic arthritis is a complex, chronic condition requiring a multidisciplinary approach for diagnosis, treatment, and long-term care. With advancements in immunomodulatory therapies and early intervention, most children can lead fulfilling lives with minimal long-term complications. Continuous education, awareness, and access to comprehensive care are pivotal in optimizing outcomes for affected individuals.