Poisoning Due to Nerve Agent: Nerve agent poisoning refers to the toxic effects caused by a group of highly lethal chemical compounds designed to disrupt the nervous system. These substances, including sarin, VX, soman, and tabun, are classified as organophosphorus compounds and are often deployed as chemical warfare agents. Exposure, even in minuscule quantities, can result in rapid onset of symptoms and death if not promptly treated.
Classification and Types of Nerve Agents
Common Nerve Agents
| Nerve Agent | Abbreviation | Volatility | Lethality | Use Case |
|---|---|---|---|---|
| Sarin | GB | High | Extremely High | Military use |
| VX | VX | Low | Highest | Persistent agent |
| Tabun | GA | Moderate | High | Early warfare agent |
| Soman | GD | Moderate | High | Battlefield use |
Characteristics of Poisoning Due to Nerve Agent
- Organophosphate structure
- Inhibit acetylcholinesterase enzyme
- Rapid absorption through skin, inhalation, and mucosa
- Persistent and non-persistent variants
Mechanism of Action: How Nerve Agents Affect the Body
Nerve agents act by irreversibly inhibiting acetylcholinesterase (AChE), the enzyme responsible for degrading acetylcholine in synaptic clefts. This results in an overaccumulation of acetylcholine, leading to continuous stimulation of muscles, glands, and the central nervous system.
Symptoms of Nerve Agent Poisoning
Muscarinic Effects (SLUDGE Syndrome)
- Salivation
- Lacrimation
- Urination
- Defecation
- Gastrointestinal upset
- Emesis
Nicotinic Effects
- Muscle fasciculations
- Paralysis
- Tachycardia or bradycardia
- Hypertension or hypotension
Central Nervous System Effects
- Headache
- Anxiety and restlessness
- Convulsions
- Coma
- Respiratory depression
Routes of Exposure
- Inhalation: Most rapid and dangerous route
- Dermal Absorption: Especially with agents like VX
- Ingestion: Rare, but highly lethal
- Ocular Contact: Causes miosis, visual disturbances
Diagnosis of Nerve Agent Poisoning
Clinical Evaluation
Diagnosis is primarily clinical, based on characteristic symptoms and known exposure history. Rapid onset of cholinergic crisis is often the first clue.
Laboratory Testing
- Cholinesterase activity measurement: Plasma (pseudocholinesterase) and RBC (true AChE)
- Detection of metabolites in blood/urine: Useful for confirmation
- Neuroimaging: May show cerebral edema or hypoxia in severe cases
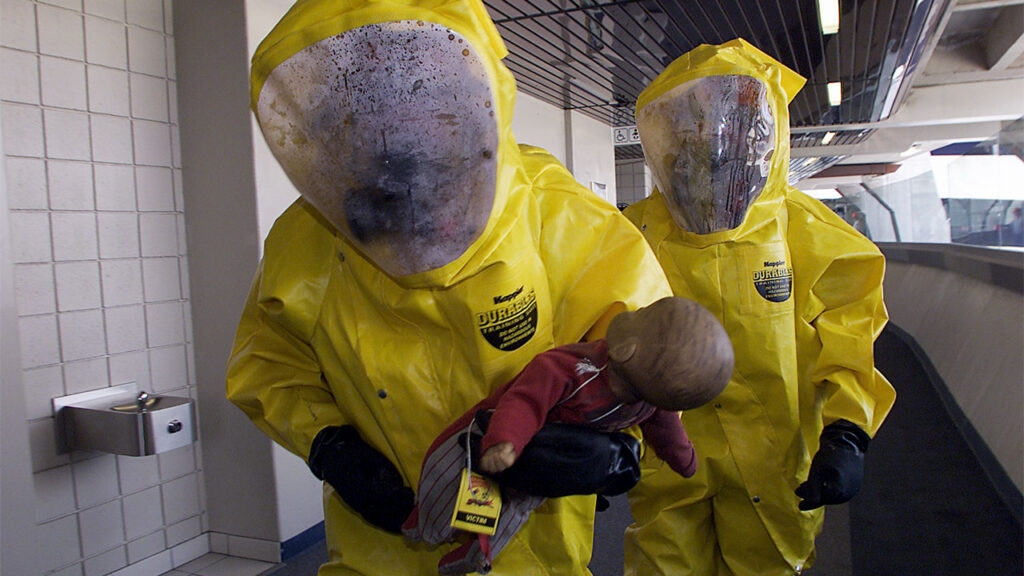
Emergency Response and Initial Management
Decontamination
- Remove clothing and rinse skin with copious amounts of water or specialized decontamination agents.
- Isolate the patient to prevent secondary contamination of healthcare providers.
- Use of personal protective equipment (PPE) for responders is essential.
Airway Management
- Ensure airway patency and oxygenation.
- Administer mechanical ventilation if respiratory failure is imminent.
Antidotal Treatment for Nerve Agent Exposure
Atropine
- Antimuscarinic agent that blocks acetylcholine effects
- Dose: 2–6 mg IV every 5–10 minutes until drying of secretions and improved respiration
Pralidoxime (2-PAM)
- Reactivates inhibited AChE before “aging” occurs
- Dose: 600–1800 mg IV over 30 minutes; repeat as needed
Diazepam or Midazolam
- For seizure control and CNS protection
- Especially critical in pediatric exposures
Medical Countermeasures and Field Protocols
Autoinjectors
- Used in battlefield or mass casualty settings
- Common configurations: Atropine + 2-PAM, sometimes with diazepam
Military and Civilian Preparedness
- Stockpiling of antidotes
- Training of emergency personnel
- Community-level response planning
Long-Term Effects and Prognosis
Neurological Sequelae
- Cognitive impairment
- Neuropathy
- Mood disorders
- Seizure disorders
Prognosis Factors
- Dose and route of exposure
- Delay in initiation of treatment
- Availability of advanced life support
- Age and underlying health conditions
Prevention and Protection Against Nerve Agents
Protective Measures
- Full-body protective suits and gas masks for personnel in risk zones
- Detection systems for airborne chemicals in military and urban areas
- Early warning networks for civil defense
Policy and Control
- Nerve agents are prohibited under the Chemical Weapons Convention (CWC)
- Controlled by international bodies such as OPCW and WHO
Frequently Asked Questions
What is the most dangerous nerve agent?
VX is considered the most lethal due to its low volatility, high persistence, and dermal absorption capabilities.
How quickly do symptoms appear after exposure?
Symptoms can begin within seconds to minutes depending on the dose and route of exposure.
Is there a vaccine for nerve agent poisoning?
No widely available vaccines exist. Prophylactic pyridostigmine is used in military settings for certain agents.
Can nerve agent poisoning be survived?
Yes, with immediate decontamination, antidote administration, and supportive care, survival is possible even after severe exposure.
What should civilians do in case of suspected nerve agent release?
Evacuate the area, remove clothing, wash exposed skin, and seek immediate medical attention.
Nerve Agent Poisoning as a Global Security Concern
Poisoning due to nerve agents remains one of the gravest threats in modern chemical warfare and terrorism. The speed and severity with which these compounds act demand rapid recognition, structured emergency protocols, and access to effective antidotes. Public health systems, emergency responders, and global policy frameworks must remain vigilant and prepared to mitigate the devastating consequences of nerve agent exposure.