Staphylococcus aureus, a gram-positive coccus, is a common cause of both community-acquired and hospital-acquired pneumonia. It is known for its aggressive nature, frequent complications, and a high incidence of antimicrobial resistance. Particularly concerning are infections caused by methicillin-resistant Staphylococcus aureus (MRSA), which necessitate urgent, targeted therapy. Pneumonia due to S. aureus often affects vulnerable individuals and can lead to rapid clinical deterioration.
Epidemiology and Risk Factors
Global Burden
Staphylococcus aureus is responsible for approximately 10–20% of bacterial pneumonias worldwide. It is a leading cause of ventilator-associated pneumonia (VAP), especially in intensive care units.
Key Risk Factors
- Recent influenza infection
- Hospitalization, especially in ICU
- Mechanical ventilation
- Chronic illnesses (diabetes, COPD, renal failure)
- Immunosuppression
- Presence of indwelling medical devices
- Previous antibiotic therapy
Transmission and Pathophysiology
Modes of Transmission
- Endogenous colonization: Nasal and skin flora can be aspirated into the lungs.
- Person-to-person spread: Via contact with contaminated surfaces or medical equipment.
- Aerosol inhalation: Especially in post-viral superinfections.
Pathophysiological Mechanism
Once in the lungs, S. aureus invades alveolar spaces, releasing cytotoxins and enzymes that destroy tissue, leading to necrotizing pneumonia. The pathogen’s ability to form biofilms and evade immune responses contributes to its severity.
Clinical Presentation of Staphylococcus aureus Pneumonia
Symptoms
- High fever with chills
- Rapid-onset cough producing purulent or bloody sputum
- Chest pain, especially pleuritic in nature
- Dyspnea and tachypnea
- Hypoxia and cyanosis in severe cases
- Altered mental status in elderly or severely ill patients
Physical Examination Findings
- Bronchial breath sounds
- Dullness to percussion over consolidation
- Crackles or rales on auscultation
- Signs of systemic toxicity and septicemia
Diagnostic Evaluation
Radiological Imaging
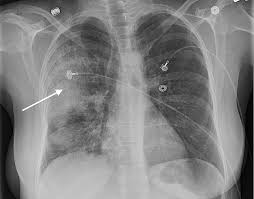
- Chest X-ray: Shows multilobar consolidation, cavitary lesions, and pneumatoceles.
- CT scan: Useful in detecting abscesses, necrosis, and empyema.
Microbiological Testing
- Sputum culture and Gram stain: Identifies gram-positive cocci in clusters.
- Blood cultures: Frequently positive in severe cases.
- Bronchoalveolar lavage (BAL): Recommended in ventilated patients.
- PCR and antigen detection tests: Aid in rapid identification and resistance profiling.
Classification of Staphylococcal Pneumonia
Methicillin-Sensitive S. aureus (MSSA) Pneumonia
- Common in both community and healthcare settings
- Typically responsive to beta-lactam antibiotics
Methicillin-Resistant S. aureus (MRSA) Pneumonia
- Frequently hospital-acquired or post-influenza
- Associated with higher morbidity, resistance to common antibiotics
- Requires specific anti-MRSA agents
Antimicrobial Management of S. aureus Pneumonia
Empirical Therapy
Initiated based on risk factors and local resistance patterns:
- MSSA: Nafcillin, oxacillin, or cefazolin
- MRSA: Vancomycin or linezolid as first-line therapy
Alternative and Adjunct Therapies
- Daptomycin (not for pulmonary use due to inactivation by lung surfactant)
- Ceftaroline for refractory MRSA
- Clindamycin for toxin suppression (e.g., PVL-producing strains)
Treatment Duration
- Uncomplicated cases: 7–10 days
- Complicated or necrotizing pneumonia: 14–21 days
Complications of Staphylococcal Pneumonia
- Lung abscesses and cavitation
- Empyema
- Pneumatoceles (especially in children)
- Septic shock
- Disseminated intravascular coagulation (DIC)
- Metastatic infections (e.g., endocarditis, osteomyelitis)
Supportive and Adjunctive Care
- Oxygen therapy or ventilatory support in respiratory failure
- Fluid and electrolyte balance
- Hemodynamic monitoring in septic patients
- Chest tube drainage for empyema
- Surgical intervention for abscesses or severe necrosis
Infection Control and Prevention
Hospital Infection Control Measures
- Rigorous hand hygiene and barrier precautions
- Decontamination of medical equipment
- Isolation protocols for MRSA-positive patients
- Decolonization protocols (e.g., mupirocin nasal ointment) in carriers
Community and Individual-Level Prevention
- Influenza vaccination to reduce post-viral pneumonia
- Early management of respiratory infections
- Awareness and control of chronic diseases
- Responsible antibiotic use to prevent resistance
Prognosis and Mortality
Pneumonia due to Staphylococcus aureus, particularly MRSA, carries a high mortality rate, reaching 30–50% in ICU settings. Early identification, aggressive management, and appropriate antimicrobial therapy are critical to improving patient outcomes.
Frequently Asked Questions:
What is the difference between MRSA and MSSA pneumonia?
MRSA is resistant to methicillin and many other beta-lactam antibiotics, requiring more specific therapy like vancomycin or linezolid, while MSSA can be treated with standard beta-lactams.
Is Staphylococcus aureus pneumonia contagious?
Yes, especially in healthcare settings through contact transmission, but it is less commonly spread through respiratory droplets.
Can pneumonia due to S. aureus occur after the flu?
Yes, secondary bacterial pneumonia due to S. aureus, particularly MRSA, is a serious complication of influenza infection.
How is MRSA pneumonia diagnosed quickly?
Rapid molecular testing (e.g., PCR) from respiratory specimens and blood can detect MRSA DNA and resistance genes promptly.
What are the signs that S. aureus pneumonia is worsening?
Worsening respiratory distress, persistent fever, septic shock, or new lung cavitations on imaging are signs of progression.
Importance of Timely Diagnosis and Targeted Therapy
Pneumonia caused by Staphylococcus aureus demands a high index of suspicion, especially in post-viral settings or hospital environments. The rising prevalence of MRSA highlights the importance of antimicrobial stewardship, early molecular diagnostics, and aggressive management. Protecting vulnerable populations through infection control and preventive strategies remains essential in mitigating the impact of this potentially fatal disease.