Klebsiella pneumoniae is a gram-negative, encapsulated bacillus commonly associated with severe hospital-acquired and community-acquired pneumonia. It is notorious for causing aggressive lung infections, particularly in immunocompromised patients, and is increasingly linked to multidrug resistance. This pathogen is capable of producing life-threatening necrotizing pneumonia, often complicated by bacteremia and lung abscesses.
Pathogenesis and Transmission of Klebsiella pneumoniae
Klebsiella pneumoniae primarily colonizes the human oropharynx and gastrointestinal tract. In immunosuppressed individuals or those with predisposing conditions, aspiration of the bacteria into the lower respiratory tract can lead to severe pneumonia.
Key Transmission Routes:
- Aspiration of oropharyngeal flora
- Contaminated hands or instruments in healthcare settings
- Endogenous spread from gut colonization
High-Risk Groups and Predisposing Factors
While Klebsiella can affect anyone, certain groups are more vulnerable due to compromised immunity or structural lung abnormalities.
Major Risk Factors Include:
- Chronic alcoholism
- Diabetes mellitus
- Chronic lung disease (COPD, bronchiectasis)
- Prolonged hospitalization or ICU stay
- Mechanical ventilation
- Use of invasive devices (e.g., catheters, ventilators)
- Immunosuppressive therapy or conditions (e.g., HIV, malignancies)
Clinical Manifestations of Klebsiella pneumoniae Pneumonia
The clinical presentation is often severe and rapidly progressive. Typical features include:
- High-grade fever with chills
- Productive cough with thick, blood-tinged or “currant jelly” sputum
- Pleuritic chest pain
- Shortness of breath
- Tachypnea and respiratory distress
- Altered mental status in elderly or critically ill patients
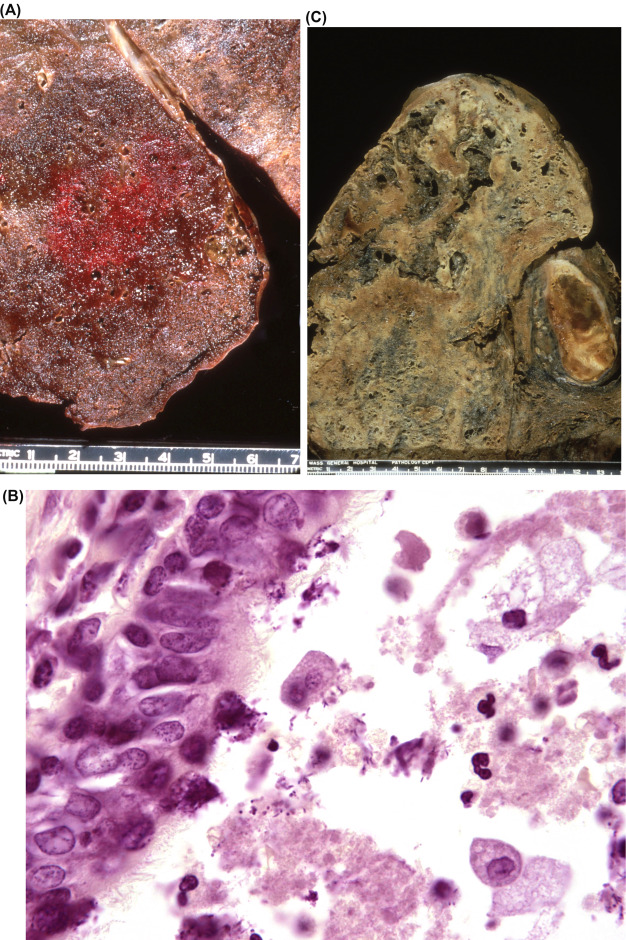
In some cases, localized lung necrosis or cavitation may be observed, distinguishing it from milder pneumonias.
Diagnostic Approach to Klebsiella pneumoniae Pneumonia
Clinical Assessment
- History of recent hospital admission, mechanical ventilation, or risk factors
- Physical signs including crackles, bronchial breath sounds, and egophony
Radiological Evaluation
- Chest X-ray: Shows lobar consolidation, cavitary lesions, and bulging fissures in severe cases
- CT Scan: Provides detailed view of lung damage, necrosis, or abscess formation
Microbiological Testing
- Sputum Gram stain and culture: Shows gram-negative rods with mucoid colonies
- Blood cultures: Essential to detect bacteremia
- Bronchoalveolar lavage (BAL): Used for deep respiratory sampling in ventilated patients
- PCR and rapid molecular diagnostics: Aid in identifying resistance genes and species-level confirmation
Antimicrobial Treatment Strategy
Due to the increasing prevalence of extended-spectrum beta-lactamase (ESBL) and carbapenem-resistant strains, treatment must be guided by sensitivity testing.
First-Line Empirical Therapy
- For non-resistant strains: Third-generation cephalosporins (e.g., ceftriaxone) or beta-lactam/beta-lactamase inhibitors
- For ESBL-producing strains: Carbapenems (e.g., meropenem, imipenem)
For Carbapenem-Resistant Klebsiella pneumoniae (CRKP)
- Polymyxins (e.g., colistin)
- Tigecycline
- Ceftazidime-avibactam
- Combination therapy often recommended
Treatment Duration
- Typically ranges from 10–14 days depending on clinical response, pathogen, and presence of complications
Management in Critical Care Settings
Patients with Klebsiella pneumoniae pneumonia often require intensive supportive measures due to respiratory failure or sepsis.
Key components of care include:
- Oxygen supplementation or ventilatory support
- Fluid resuscitation for septic shock
- Vasopressors in hemodynamic instability
- Close monitoring of renal and hepatic function
Potential Complications of K. pneumoniae Pneumonia
Due to its virulence, Klebsiella pneumoniae can lead to a spectrum of serious complications:
- Pulmonary necrosis and abscess formation
- Empyema (pus in pleural cavity)
- Sepsis and septic shock
- Acute respiratory distress syndrome (ARDS)
- Multisystem organ failure
Prompt recognition and aggressive management are vital to reduce morbidity and mortality.
Preventive Strategies Against Klebsiella pneumoniae Infection
Infection Control in Healthcare Settings
- Strict hand hygiene and use of personal protective equipment
- Sterilization of invasive devices and respiratory equipment
- Isolation protocols for patients with multidrug-resistant infections
- Antimicrobial stewardship programs to reduce antibiotic resistance
Community and Individual-Level Measures
- Control of diabetes and other chronic illnesses
- Smoking and alcohol cessation
- Pneumococcal and influenza vaccination to reduce secondary infections
- Minimizing unnecessary antibiotic usage
Prognosis and Outcome
The mortality rate of pneumonia due to Klebsiella pneumoniae can be high, particularly in those with multidrug-resistant infections or delayed treatment. Mortality exceeds 50% in severe cases with bacteremia or sepsis. Early recognition, tailored antibiotic therapy, and critical care interventions significantly improve survival.
Frequently Asked Questions:
What makes Klebsiella pneumoniae so dangerous in pneumonia?
Its thick capsule resists phagocytosis, and many strains produce ESBL or carbapenemases, rendering them resistant to multiple antibiotics.
Is Klebsiella pneumoniae pneumonia contagious?
While person-to-person spread is rare in the community, it is transmissible in hospitals through contaminated surfaces and hands.
Can Klebsiella pneumoniae be part of the normal flora?
Yes, it commonly resides in the gastrointestinal tract without causing harm unless it gains access to sterile sites.
How can multidrug-resistant strains be identified?
Through antimicrobial susceptibility testing and molecular diagnostics like PCR to detect resistance genes.
Is there a vaccine for Klebsiella pneumoniae?
Currently, there is no licensed vaccine, but research is ongoing to develop one, especially targeting high-risk populations.
Urgency in Addressing Klebsiella-Linked Pneumonia
Pneumonia caused by Klebsiella pneumoniae remains a formidable clinical challenge due to its rapid progression, high virulence, and increasing resistance. A combination of early diagnosis, targeted antimicrobial therapy, and robust infection control practices is essential to combat this pathogen. Continued surveillance, antibiotic stewardship, and advancements in vaccine development will be key in mitigating its global health impact.