Pneumocystis jirovecii pneumonia (PJP), formerly known as Pneumocystis carinii pneumonia (PCP), is a life-threatening opportunistic infection caused by the atypical fungal organism Pneumocystis jirovecii. It predominantly affects immunocompromised individuals, particularly those with HIV/AIDS, malignancies, organ transplants, or those on immunosuppressive therapy. PJP is one of the most common AIDS-defining illnesses and remains a critical cause of morbidity and mortality among immunosuppressed populations.
Pathogenesis and Transmission of Pneumocystis Jirovecii
P. jirovecii is an obligate extracellular organism with fungal characteristics but lacks ergosterol, making its treatment unique among fungal infections. Its primary mode of transmission is airborne, through inhalation of cysts or trophic forms.
In immunocompetent individuals, the immune system clears the organism effectively. In contrast, immunosuppressed patients cannot mount an adequate response, leading to alveolar inflammation and impaired gas exchange.
Risk Factors and Populations at Risk
PJP can occur in a wide array of immunocompromised hosts. The risk is particularly elevated in:
- HIV/AIDS patients with CD4+ T-cell counts <200 cells/μL
- Solid organ transplant recipients, especially within the first 6 months post-transplant
- Patients on corticosteroids ≥20 mg/day prednisone equivalent for >4 weeks
- Patients receiving chemotherapy or TNF-α inhibitors
- Hematologic malignancy patients and those undergoing stem cell transplant
Subclinical colonization in immunocompetent individuals has been documented, highlighting the potential for asymptomatic transmission.
Clinical Features and Symptomatology
The presentation of PJP differs significantly between HIV-positive and HIV-negative individuals.
In HIV-positive patients:
- Gradual onset over days to weeks
- Low-grade fever
- Non-productive dry cough
- Progressive exertional dyspnea
- Weight loss and night sweats
In HIV-negative immunocompromised patients:
- Rapid onset respiratory failure
- High-grade fever
- Tachypnea and hypoxia
- Cough may be absent
Auscultation is often unremarkable, despite severe hypoxemia, leading to clinical-radiologic dissociation.
Radiological and Laboratory Diagnosis
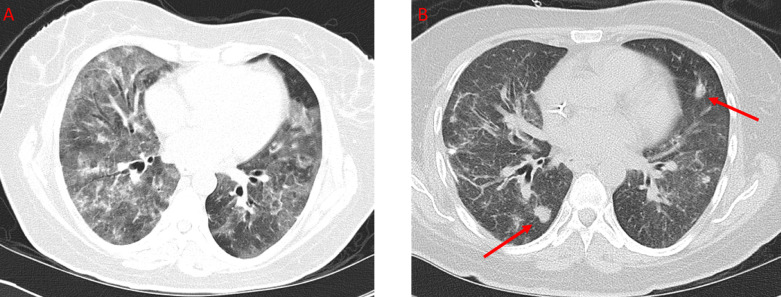
Imaging Studies:
- Chest X-ray: Bilateral interstitial infiltrates; may be normal early in disease
- High-resolution CT (HRCT): Ground-glass opacities, perihilar distribution, cystic lesions in advanced disease
Laboratory and Microbiological Testing:
- Arterial Blood Gas (ABG): Hypoxemia with increased alveolar-arterial gradient
- LDH levels: Elevated (>500 IU/L), nonspecific but commonly seen
- Beta-D-glucan assay: Elevated in most fungal infections including PJP
- PCR testing: High sensitivity but can detect colonization
- Direct Fluorescent Antibody (DFA) staining: Gold standard for organism detection in induced sputum or BAL
- Bronchoalveolar Lavage (BAL): Highest diagnostic yield, especially in non-HIV patients
Histopathology and Microscopic Identification
On histologic examination, Pneumocystis organisms appear as:
- Cysts: Thick-walled, cup-shaped structures with intracystic bodies
- Trophic forms: Smaller and difficult to visualize without special stains
- Common stains: Gomori methenamine silver (GMS), toluidine blue, or calcofluor white
Management and Treatment Strategies
First-Line Therapy:
- Trimethoprim-Sulfamethoxazole (TMP-SMX): 15–20 mg/kg/day of TMP divided in 3–4 doses IV or oral
- Duration: 21 days in HIV-positive patients; 14 days in non-HIV patients
Alternative Agents (for TMP-SMX intolerance):
- Pentamidine (IV) – Reserved for severe cases
- Atovaquone (oral) – For mild to moderate disease
- Clindamycin + Primaquine – Effective for moderate to severe PJP
- Dapsone + Trimethoprim – Alternative for mild cases
Adjunctive Therapy:
- Corticosteroids: Indicated in patients with PaO₂ <70 mmHg or A-a gradient >35 mmHg
- Prednisone 40 mg twice daily for 5 days, then taper
- Reduces risk of respiratory failure and death in HIV-associated PJP
Supportive Care:
- Oxygen supplementation
- Mechanical ventilation in ARDS
- Avoid nephrotoxic medications during treatment
Prophylaxis and Prevention
Indications for Primary Prophylaxis:
- HIV patients with CD4 count <200 cells/μL
- Patients on immunosuppressive therapy (e.g., post-transplant or chemotherapy)
- Those with history of PJP
Preferred Prophylactic Regimen:
- TMP-SMX: 1 double-strength tablet daily or 3 times/week
- Alternatives: Dapsone, Atovaquone, or aerosolized Pentamidine
Vaccination and early initiation of ART in HIV patients are key components of prevention strategies.
Prognosis and Outcomes
PJP mortality is significantly influenced by host immune status:
- HIV-positive patients: Mortality rates 10–20% with appropriate treatment
- Non-HIV patients: Higher mortality (30–50%) due to acute onset and delayed diagnosis
- Poor prognostic indicators include:
- Late treatment initiation
- Severe hypoxemia
- Mechanical ventilation requirement
- Co-infections or neutropenia
Antifungal Resistance and Research Directions
While resistance to TMP-SMX is rare, mutations in dhps and dhfr genes have been identified and associated with clinical failure. Ongoing studies are evaluating:
- Novel antifungal agents targeting folate biosynthesis pathways
- Inhaled therapies for localized lung delivery
- Host-directed therapies to mitigate inflammatory lung damage
Frequently Asked Questions:
What is Pneumocystis jirovecii pneumonia?
It is a serious lung infection caused by the fungus Pneumocystis jirovecii, primarily affecting immunocompromised individuals.
Who is most at risk for PJP?
HIV-positive individuals with low CD4 counts, transplant recipients, cancer patients, and those on prolonged immunosuppressive drugs.
How is PJP diagnosed?
Through chest imaging, laboratory markers like LDH and beta-D-glucan, and microscopic examination of sputum or BAL fluid.
What is the standard treatment?
Trimethoprim-Sulfamethoxazole for 14–21 days, with corticosteroids added in moderate to severe cases.
Can PJP be prevented?
Yes, with prophylactic antibiotics such as TMP-SMX and immune reconstitution via ART in HIV patients.
Is it contagious?
Transmission occurs through airborne routes, but person-to-person spread is not well established in clinical settings.