Pneumococcus endocarditis, a rare yet life-threatening form of infective endocarditis, is caused by Streptococcus pneumoniae. Despite the organism’s well-known role in pneumonia and meningitis, its involvement in endocardial infections represents a particularly aggressive and fulminant clinical entity. Historically more common before the antibiotic era, pneumococcal endocarditis now primarily affects high-risk individuals and remains a critical diagnostic consideration due to its rapid progression and high complication rate.
Pathogenesis and Microbiological Characteristics
Streptococcus pneumoniae is a gram-positive, encapsulated diplococcus capable of causing invasive disease through its virulence factors, including polysaccharide capsule, pneumolysin, and surface adhesins. In the context of endocarditis, hematogenous dissemination during pneumococcal bacteremia allows bacterial colonization of damaged or prosthetic heart valves.
The formation of bulky vegetations on the mitral or aortic valves often leads to acute valve dysfunction, septic emboli, and hemodynamic collapse.
Epidemiology and Risk Factors
Although rare, pneumococcus accounts for 1–3% of all cases of infective endocarditis. Risk factors include:
- Advanced age
- Chronic alcoholism
- Pre-existing valvular heart disease
- Prosthetic heart valves
- Immunosuppressive conditions
- Invasive pneumococcal disease (IPD)
- History of recent pneumonia, meningitis, or otitis media
Nosocomial and community-acquired sources have both been documented, with increasing reports in the context of antimicrobial resistance.
Clinical Presentation and Signs of Pneumococcal Endocarditis
The clinical course of pneumococcal endocarditis is typically acute, with rapid deterioration.
Cardinal Symptoms:
- High-grade persistent fever
- Chills and malaise
- New or changing heart murmur
- Pleuritic chest pain or dyspnea
- Neurological deficits (from embolic strokes)
Physical Findings:
- Osler’s nodes, Janeway lesions (rare in pneumococcal cases)
- Splenomegaly
- Petechiae
- Signs of congestive heart failure
- Signs of embolic phenomena: renal infarcts, cerebral emboli, splenic abscess
Multiorgan failure may develop within days if left untreated, underscoring the need for early recognition.
Diagnostic Evaluation and Laboratory Workup
Diagnosis relies on a combination of clinical suspicion, microbiological confirmation, and imaging.
Blood Cultures:
- Essential for pathogen identification
- Usually show growth of S. pneumoniae in multiple samples
- Rapid positivity due to high bacterial load
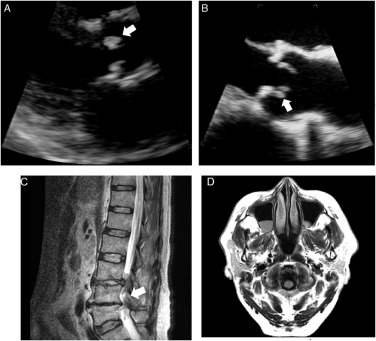
Echocardiography:
- Transthoracic Echocardiography (TTE): Initial imaging modality
- Transesophageal Echocardiography (TEE): Higher sensitivity, critical for detecting vegetations, abscesses, and prosthetic valve involvement
Modified Duke Criteria:
Incorporated in diagnostic evaluation, combining microbiological, imaging, and clinical data to confirm endocarditis.
Additional Investigations:
- CBC: Leukocytosis with neutrophilia
- ESR/CRP: Elevated
- Urinalysis: Hematuria, proteinuria (suggestive of embolic phenomena)
- CT/MRI brain: To detect septic emboli or infarcts
Complications of Pneumococcal Endocarditis
Pneumococcus-induced endocarditis is notable for its high complication rate:
- Acute heart failure due to valve destruction
- Septic emboli to the brain, spleen, or kidneys
- Perivalvular abscesses and fistula formation
- Myocardial infarction from coronary embolism
- Stroke and encephalopathy
- Mortality rates up to 30% despite therapy
Prompt surgical and medical intervention is often required to prevent irreversible damage.
Medical and Surgical Management
The cornerstone of treatment is a combination of bactericidal antibiotics and surgical valve intervention in selected cases.
Antibiotic Therapy:
Initiated immediately after obtaining blood cultures and guided by sensitivity data.
First-Line Regimens:
- Ceftriaxone 2g IV daily (or Cefotaxime)
- Vancomycin added if resistance or penicillin allergy suspected
- Duration: Minimum 4–6 weeks of intravenous therapy
Combination therapy with gentamicin has been used in select cases, although not routinely recommended due to nephrotoxicity.
Surgical Indications:
Urgent surgery may be necessary for:
- Refractory heart failure due to valve insufficiency
- Uncontrolled infection or abscess
- Large vegetations (>10 mm) with embolic events
- Prosthetic valve involvement
Supportive Care:
- Hemodynamic support in intensive care settings
- Monitoring for arrhythmias and organ dysfunction
- Rehabilitation post-infection for stroke or embolic complications
Prognosis and Outcome
The prognosis depends on timely diagnosis, virulence of the organism, extent of cardiac involvement, and presence of embolic complications.
- Mortality without treatment approaches 100%
- With optimal therapy, survival rates improve, though recurrence risk remains if underlying valve pathology is not addressed
- Surgical intervention significantly enhances long-term outcomes
Prevention and Vaccination Strategies
Given the severity of pneumococcal endocarditis, prevention of primary pneumococcal infections through vaccination is critical.
Recommended Vaccines:
- PCV13/PCV15/PCV20 (Conjugate Vaccines): Target children, elderly, and high-risk adults
- PPSV23 (Polysaccharide Vaccine): For broader serotype coverage in older adults and immunocompromised
Additional Preventive Measures:
- Prompt treatment of pneumococcal infections (e.g., pneumonia, sinusitis)
- Antibiotic prophylaxis not routinely used but may be considered in select high-risk valve patients undergoing invasive procedures
- Improved hygiene and smoking cessation
Antimicrobial Resistance Trends
Rising penicillin and macrolide resistance in S. pneumoniae has complicated empirical therapy. Surveillance data indicate geographic variability in susceptibility patterns, emphasizing the importance of local antibiograms.
- Multidrug-resistant strains are emerging due to overuse of broad-spectrum antibiotics
- Continuous vaccine development is essential to adapt to evolving serotype prevalence and resistance
Frequently Asked Questions
What is pneumococcus endocarditis?
It is an acute infection of the heart valves caused by Streptococcus pneumoniae, characterized by rapid onset and systemic complications.
How does pneumococcal endocarditis differ from other types?
It progresses more aggressively and often involves left-sided native valves with a high risk of embolization and valve destruction.
What is the mortality rate of pneumococcal endocarditis?
Even with treatment, mortality can reach 30%, particularly in older adults or those with comorbidities.
Is surgery always required?
Not in all cases, but surgical intervention is often necessary for structural valve damage, large vegetations, or uncontrolled infection.
Can it be prevented?
Yes, through pneumococcal vaccination and early treatment of invasive pneumococcal diseases.
Is it common in prosthetic valves?
While rare, prosthetic valves are susceptible and associated with higher complication rates.