Pneumococcal pharyngitis refers to a bacterial infection of the pharynx caused by Streptococcus pneumoniae. Although this pathogen is more commonly associated with pneumonia, sinusitis, and meningitis, it can also be an etiological agent in upper respiratory tract infections, including pharyngitis. The condition typically manifests as a sore throat accompanied by systemic symptoms and may be indistinguishable from other bacterial causes of pharyngitis without microbiological confirmation.
Etiology and Pathogenesis
Streptococcus pneumoniae is a gram-positive, alpha-hemolytic diplococcus that colonizes the human nasopharynx. Under specific conditions, such as weakened host immunity or mucosal barrier disruption, it can invade the pharyngeal tissues and initiate an inflammatory response.
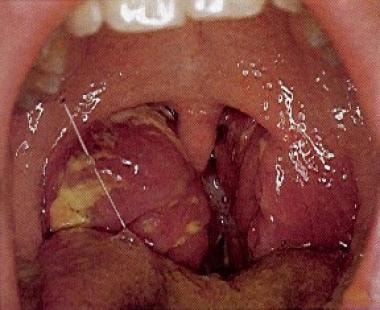
Unlike viral pharyngitis, pneumococcal pharyngitis is characterized by localized purulence and systemic signs of bacterial infection.
Clinical Presentation and Symptoms
Pneumococcal pharyngitis shares many features with other bacterial sore throats but may be accompanied by unique indicators of pneumococcal involvement.
Common symptoms include:
- Acute sore throat
- Painful swallowing (odynophagia)
- Erythematous and swollen pharynx
- Tonsillar exudates or pus
- Fever ≥ 38.5°C (101.3°F)
- Cervical lymphadenopathy
- Headache and fatigue
- Malaise or myalgia
In some cases, co-infections or superinfections may be present, complicating the diagnosis and increasing severity.
Differential Diagnosis
Differentiating pneumococcal pharyngitis from other causes is essential for targeted treatment. Key differential diagnoses include:
- Group A Streptococcal Pharyngitis (GAS)
- Viral Pharyngitis (e.g., Epstein-Barr virus, adenovirus, rhinovirus)
- Diphtheria
- Gonococcal Pharyngitis
- Mycoplasma or Chlamydial Infections
Laboratory testing is critical in accurately identifying S. pneumoniae as the causative organism.
Diagnostic Methods
Prompt and accurate diagnosis enhances treatment outcomes and limits complications. The diagnostic approach includes:
- Throat Swab Culture:
- Gold standard for identifying S. pneumoniae
- Requires blood agar culture and optochin sensitivity testing
- Rapid Antigen Detection Test (RADT):
- Generally used for GAS but not specific for pneumococci
- PCR Assays:
- Sensitive molecular tests for detecting pneumococcal DNA
- Useful in differentiating colonization from true infection
- Complete Blood Count (CBC):
- May show elevated white blood cells with a neutrophilic predominance
- Procalcitonin Levels:
- Helpful in distinguishing bacterial from viral infections
Treatment Protocols for Pneumococcal Pharyngitis
Antibiotic therapy is indicated for confirmed or strongly suspected cases of pneumococcal pharyngitis. Treatment aims to reduce symptom severity, prevent complications, and limit transmission.
First-line antibiotics:
- Amoxicillin:
Preferred due to its efficacy and safety profile - Penicillin V:
Traditional choice, especially in non-allergic patients - Cefuroxime or Cefdinir:
For beta-lactam-resistant strains or in recurrent infections - Macrolides (e.g., Azithromycin):
Alternative for penicillin-allergic individuals
Duration:
A 7–10 day course is generally recommended, with close monitoring for symptom resolution.
Complications and Sequelae
Although typically self-limited with appropriate treatment, untreated or severe pneumococcal pharyngitis may lead to complications such as:
- Peritonsillar abscess
- Otitis media
- Sinusitis
- Cervical lymphadenitis
- Pneumonia or invasive pneumococcal disease (IPD)
- Bacteremia in immunocompromised hosts
Early recognition and intervention are crucial in avoiding these outcomes.
Preventive Measures and Vaccination
Vaccination plays a vital role in reducing the incidence of pneumococcal infections, including pharyngitis.
Recommended vaccines include:
- Pneumococcal Conjugate Vaccines (PCV13, PCV15, PCV20):
Administered to infants, older adults, and at-risk populations - Pneumococcal Polysaccharide Vaccine (PPSV23):
For individuals over 65 or those with chronic medical conditions
Additional preventive strategies:
- Practicing good hand hygiene
- Avoiding close contact with symptomatic individuals
- Prompt treatment of respiratory symptoms
- Immunizing close contacts of vulnerable populations
Epidemiology and At-Risk Populations
While pharyngitis caused by S. pneumoniae is less common than that caused by Group A Streptococcus, it poses a heightened risk in certain populations:
- Children under 5 years
- Elderly adults
- Individuals with chronic respiratory disease
- Immunosuppressed patients (e.g., HIV, chemotherapy recipients)
- Smokers and individuals with asthma or COPD
Surveillance data indicate sporadic community outbreaks, especially in environments with poor vaccination uptake or crowded conditions.
Research Developments and Resistance Patterns
The global rise of antibiotic-resistant S. pneumoniae strains underscores the importance of antimicrobial stewardship. Resistance to macrolides, beta-lactams, and tetracyclines has been documented in various regions, prompting the need for routine susceptibility testing and vaccination coverage expansion.
Research continues on next-generation vaccines with broader serotype protection, rapid diagnostics to distinguish colonization from infection, and novel therapeutics for resistant strains.
Frequently Asked Questions
What bacteria causes pneumococcal pharyngitis?
Pneumococcal pharyngitis is caused by Streptococcus pneumoniae, a gram-positive, encapsulated diplococcus.
Is pneumococcal pharyngitis contagious?
Yes, it spreads via respiratory droplets from coughing, sneezing, or close contact.
How is pneumococcal pharyngitis different from strep throat?
While both are bacterial pharyngitis, strep throat is caused by Group A Streptococcus, whereas pneumococcal pharyngitis is due to S. pneumoniae.
Can pneumococcal pharyngitis lead to serious illness?
If untreated, it may lead to complications such as abscess formation, sinusitis, or even invasive diseases.
Is there a vaccine for pneumococcal pharyngitis?
No vaccine targets pharyngitis specifically, but pneumococcal vaccines can reduce overall S. pneumoniae infections.
Should antibiotics be used for every sore throat?
No. Only confirmed or suspected bacterial infections like pneumococcal or strep throat warrant antibiotic therapy.