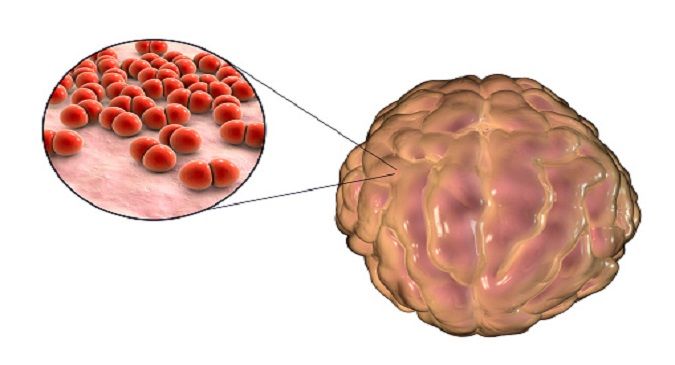
Pneumococcal meningitis is a life-threatening bacterial infection of the membranes (meninges) surrounding the brain and spinal cord. Caused by Streptococcus pneumoniae, this condition is a form of invasive pneumococcal disease (IPD) and is most prevalent in infants, elderly individuals, and immunocompromised populations. Left untreated, it can lead to serious complications including brain damage, hearing loss, and death.
Pathophysiology and Transmission
Streptococcus pneumoniae colonizes the nasopharynx and can invade the bloodstream, eventually reaching the central nervous system. Upon entering the meninges, it triggers an intense inflammatory response, disrupting the blood-brain barrier and increasing intracranial pressure.
Transmission occurs through respiratory droplets, making close-contact environments such as schools, daycare centers, and nursing homes particularly vulnerable to outbreaks.
Signs and Symptoms of Pneumococcal Meningitis
Symptoms can develop rapidly, often within hours of infection. Clinical presentation varies by age, but common signs include:
- Adults and Older Children:
- Sudden high fever
- Severe headache
- Neck stiffness
- Sensitivity to light (photophobia)
- Altered mental status or confusion
- Seizures
- Infants and Young Children:
- Bulging fontanelle
- Irritability or lethargy
- Poor feeding
- Vomiting
- Hypotonia
Prompt recognition of these symptoms is crucial for timely medical intervention.
Risk Factors and Vulnerable Populations
Certain groups are at elevated risk for pneumococcal meningitis, including:
- Children under 5 years, especially under 2
- Adults over 65 years
- Individuals with cochlear implants
- People with cerebrospinal fluid leaks
- Immunocompromised individuals (e.g., HIV/AIDS, cancer, splenectomy)
- Those with chronic diseases (e.g., diabetes, alcoholism)
Vaccination and targeted preventive care are essential for these high-risk groups.
Diagnosis and Laboratory Testing
Early diagnosis is vital. Diagnostic procedures include:
- Lumbar Puncture (Spinal Tap):
Collects cerebrospinal fluid (CSF) for laboratory analysis. Findings typically reveal:- Elevated white blood cell count
- Increased protein levels
- Decreased glucose concentration
- Positive Gram stain for gram-positive diplococci
- Blood Cultures:
Helpful in identifying bacteremia associated with the infection. - Polymerase Chain Reaction (PCR):
Highly sensitive method to detect pneumococcal DNA in CSF samples. - Imaging (CT/MRI):
Used to rule out contraindications before lumbar puncture and identify complications such as brain abscess or hydrocephalus.
Effective Treatment Strategies
Prompt administration of empiric intravenous antibiotics is critical. Treatment protocol typically includes:
- First-Line Antibiotics:
- Ceftriaxone or cefotaxime
- Vancomycin (to cover resistant strains)
- Addition of dexamethasone may reduce neurological complications if administered early
- Tailored Therapy: Adjusted based on susceptibility testing of isolated strains.
- Supportive Care: Management of complications like seizures, increased intracranial pressure, or respiratory distress may require ICU-level monitoring.
Complications and Long-Term Effects
Despite advances in medical care, pneumococcal meningitis is associated with high morbidity and mortality rates. Potential complications include:
- Permanent hearing loss
- Intellectual disability
- Epilepsy
- Hydrocephalus
- Limb amputation in severe cases with sepsis
Survivors, particularly children, may require long-term rehabilitation and support services.
Prevention: Vaccination and Public Health Measures
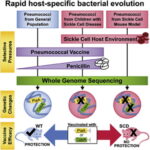
Vaccination remains the most effective preventive strategy:
- Pneumococcal Conjugate Vaccine (PCV13 or PCV15):
Recommended for all infants, adults over 65, and high-risk groups. - Pneumococcal Polysaccharide Vaccine (PPSV23):
Administered to adults over 65 and individuals with certain health conditions.
Public health efforts also include:
- Ensuring high vaccine coverage
- Promoting hand hygiene
- Educating at-risk populations
- Preventing overcrowded living conditions
Global Burden and Epidemiology
Pneumococcal meningitis contributes significantly to global meningitis-related deaths, particularly in low-income countries with limited access to vaccines and healthcare infrastructure. According to WHO data, the incidence has decreased significantly in countries with comprehensive immunization programs, yet it remains a public health challenge in under-vaccinated regions.
Research and Future Outlook
Ongoing research focuses on:
- Development of broader-spectrum pneumococcal vaccines
- Understanding antimicrobial resistance patterns
- Enhancing rapid diagnostic techniques
- Implementing global strategies for vaccine equity
As we continue to advance in vaccine technology and public health policies, the burden of pneumococcal meningitis can be further reduced globally.