Pneumococcal Infection Prevention in Sickle Cell Disease: Sickle cell disease (SCD) significantly increases vulnerability to pneumococcal infections, particularly invasive pneumococcal disease (IPD) such as bacteremia, sepsis, and meningitis. The spleen, essential in filtering bacteria like Streptococcus pneumoniae, becomes functionally impaired or auto-infarcted early in life in individuals with SCD. This functional asplenia compromises immune defense, placing patients at high risk for rapid and fatal pneumococcal infections.
Without proper prevention, pneumococcal infections in SCD can lead to swift deterioration and death, often within 24 to 48 hours of symptom onset.
Pathophysiology: Why SCD Patients Are More Vulnerable
In sickle cell disease, repeated sickling of red blood cells obstructs splenic blood flow. This ischemia results in progressive splenic infarction and eventually functional asplenia, which typically develops by age 5. The absence of spleen-mediated immune surveillance critically weakens the ability to clear encapsulated bacteria, particularly Streptococcus pneumoniae.
Key Strategies for Pneumococcal Infection Prevention in SCD
1. Pneumococcal Vaccination Protocol
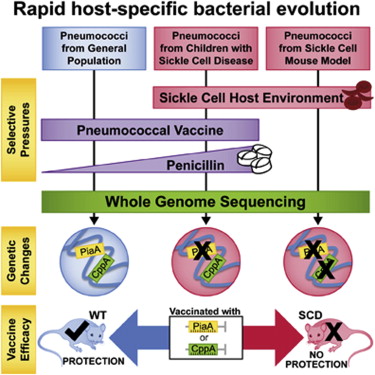
Vaccination is the cornerstone of pneumococcal infection prevention in individuals with sickle cell disease.
a. Pneumococcal Conjugate Vaccine (PCV13 or PCV15)
- Initiated at 2 months of age
- Subsequent doses at 4, 6, and 12–15 months
- Provides immunity against common invasive serotypes
- Induces strong T-cell-dependent responses
b. Pneumococcal Polysaccharide Vaccine (PPSV23)
- Administered at 2 years of age
- Booster given 5 years later
- Covers broader serotype range not included in PCV13
c. Newer Options: PCV20
- May be recommended in future schedules for broader coverage
Recommended Vaccine Schedule for SCD Patients:
| Age | Vaccine | Notes |
|---|---|---|
| 2, 4, 6 months | PCV13/PCV15 | Primary doses |
| 12–15 months | PCV13/PCV15 | Booster |
| 2 years | PPSV23 | First polysaccharide vaccine |
| 7 years | PPSV23 | Booster if previously vaccinated |
2. Penicillin Prophylaxis
Continuous antibiotic prophylaxis significantly reduces pneumococcal infection rates in young children with SCD.
a. Initiation and Dosage
- Start at 2 months of age
- Penicillin V potassium: 125 mg orally twice daily (under 3 years); 250 mg twice daily (over 3 years)
b. Duration
- Recommended through at least 5 years of age
- Lifelong prophylaxis may be considered in patients with prior IPD or documented asplenia
c. Alternative
- Erythromycin for penicillin-allergic individuals
3. Parent and Caregiver Education
Educating families is vital to ensure timely vaccination and medication adherence.
Key topics include:
- Recognizing early signs of pneumococcal infection (fever, lethargy, irritability)
- Importance of immediate medical attention for febrile episodes
- Adherence to prophylaxis and routine healthcare follow-ups
4. Prompt Medical Evaluation for Febrile Illness
Children with SCD presenting with fever ≥38.5°C (101.3°F) require urgent medical evaluation and empirical antibiotics.
Empirical therapy includes:
- Ceftriaxone or cefotaxime
- Blood cultures and laboratory testing
- Hospitalization for close observation, especially under age 3
5. Surveillance and Long-Term Follow-Up
Ongoing care involves monitoring vaccine response and updating prophylactic measures.
- Annual influenza vaccination to prevent secondary bacterial pneumonia
- Re-vaccination with PPSV23 after 5 years
- Assessment of antibody titers if clinically indicated
Impact of Preventive Strategies on Health Outcomes
Studies have consistently shown that pneumococcal vaccination and penicillin prophylaxis dramatically reduce the incidence of IPD in SCD patients:
- 90% reduction in IPD rates since the introduction of PCV13
- Early penicillin prophylaxis reduces mortality in children under five
- Herd immunity offers indirect protection, but individual vaccination remains essential
Global Recommendations and Guidelines
Centers for Disease Control and Prevention (CDC)
- Endorses universal pneumococcal vaccination in SCD
- Recommends lifelong vigilance and prophylaxis for high-risk individuals
American Academy of Pediatrics (AAP)
- Emphasizes early initiation of penicillin and strict adherence to vaccine schedules
WHO Position
- Advocates inclusion of pneumococcal vaccines in national immunization programs
- Recommends prioritization for children with hemoglobinopathies
Challenges in Implementation and Solutions
| Challenge | Solution |
|---|---|
| Limited access to healthcare in low-income regions | Mobile clinics and community health initiatives |
| Non-adherence to prophylaxis | Enhanced caregiver education and digital reminder systems |
| Vaccine hesitancy | Outreach campaigns emphasizing vaccine safety and success |
Pneumococcal infection prevention in sickle cell disease requires a multi-faceted, lifelong approach combining vaccination, antibiotic prophylaxis, education, and proactive healthcare. With strict adherence to current guidelines and improved healthcare access, we can drastically reduce morbidity and mortality in this vulnerable population.