Pneumococcal acute otitis media (AOM) is a common and potentially severe infection of the middle ear, primarily caused by Streptococcus pneumoniae. It is especially prevalent among infants and young children and is a leading cause of antibiotic prescriptions in pediatric practice. This condition contributes significantly to healthcare utilization worldwide and presents a considerable public health burden.
Pathophysiology of Streptococcus pneumoniae in Otitis Media
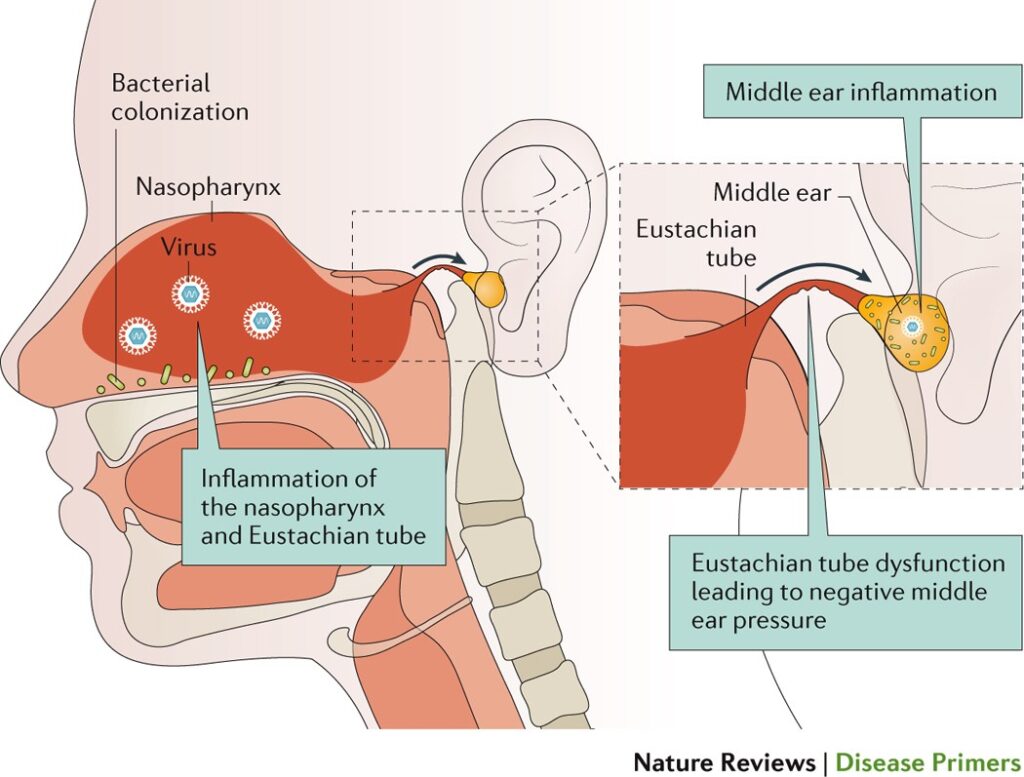
The pathogenesis of pneumococcal AOM typically begins with a preceding upper respiratory tract infection, which leads to eustachian tube dysfunction and impaired middle ear ventilation. This environment allows for the invasion and proliferation of S. pneumoniae, resulting in inflammation and fluid accumulation within the middle ear.
The bacterial infection elicits an inflammatory response that leads to otalgia (ear pain), fever, irritability, and potentially hearing loss.
Epidemiology and Risk Factors
Acute otitis media caused by Streptococcus pneumoniae predominantly affects children under the age of five. The following factors increase the risk:
- Age below 2 years
- Attendance at daycare centers
- Lack of breastfeeding
- Exposure to tobacco smoke
- Seasonal variation (peaks in winter and early spring)
- Family history of recurrent ear infections
- Anatomical abnormalities (e.g., cleft palate)
Clinical Presentation of Pneumococcal AOM
The signs and symptoms of pneumococcal AOM are often abrupt and include:
- Ear pain (otalgia), often severe
- Fever, typically >38°C
- Irritability or crying, especially in infants
- Hearing loss or muffled sounds
- Tugging or pulling at the ear
- Otorrhea in cases of tympanic membrane perforation
In preverbal children, non-specific symptoms such as poor feeding, sleep disturbances, and inconsolable crying may predominate.
Diagnosis of Pneumococcal Acute Otitis Media
Otoscopic Examination
Diagnosis is primarily clinical, based on:
- Bulging of the tympanic membrane
- Middle ear effusion
- Reduced tympanic membrane mobility on pneumatic otoscopy
- Purulent otorrhea in the absence of otitis externa
Laboratory Testing
While not routinely required, culture of middle ear fluid obtained by tympanocentesis confirms the presence of S. pneumoniae. This is reserved for:
- Severe or recurrent cases
- Treatment failures
- Infants under 6 months
Rapid antigen detection and PCR assays are emerging as sensitive diagnostic alternatives in research settings.
Antimicrobial Management and Treatment Guidelines
First-Line Therapy
- Amoxicillin (high dose: 80–90 mg/kg/day) is the first-line antibiotic due to its efficacy against S. pneumoniae.
- In cases of β-lactam allergy: Cefdinir, Cefuroxime, or Azithromycin may be used.
Duration of Therapy
- 10 days for children under 2 years or with severe disease
- 5–7 days for older children with mild or moderate illness
Criteria for Watchful Waiting
Observation without immediate antibiotics may be appropriate in:
- Children >2 years with mild symptoms
- Unilateral AOM without otorrhea
Close follow-up is necessary to initiate antibiotics if symptoms worsen.
Complications of Pneumococcal AOM
If inadequately treated, pneumococcal AOM may lead to complications including:
- Tympanic membrane perforation
- Otitis media with effusion (OME)
- Hearing impairment
- Mastoiditis
- Meningitis
- Intracranial abscess (rare)
Early recognition and intervention are crucial to prevent such sequelae.
Prevention: Role of Pneumococcal Vaccination
The pneumococcal conjugate vaccine (PCV13) has dramatically reduced the incidence of AOM caused by vaccine-covered serotypes of S. pneumoniae. Additional strategies include:
- Annual influenza vaccination: reduces the risk of viral URTIs that predispose to AOM
- Breastfeeding: for at least 6 months
- Avoidance of tobacco smoke exposure
- Appropriate hand hygiene in daycare and school environments
Impact of Vaccination
Since the introduction of PCV7 and later PCV13, there has been:
- A significant decline in pneumococcal AOM cases
- Shift in serotype distribution (serotype replacement)
- Reduced antibiotic resistance due to decreased overall antibiotic use
Management of Recurrent and Chronic Otitis Media
Recurrent AOM
Defined as:
- ≥3 episodes in 6 months or
- ≥4 episodes in 12 months with one in the past 6 months
Management includes:
- Prophylactic antibiotics (controversial)
- Tympanostomy tube placement
- Adenoidectomy in selected cases
Otitis Media with Effusion (OME)
This is a common sequela characterized by persistent middle ear effusion without acute infection symptoms. Observation is recommended initially, with surgical intervention if effusion persists beyond 3 months or causes hearing loss.
Pneumococcal acute otitis media remains a leading cause of morbidity among young children. Prompt diagnosis and appropriate antibiotic therapy ensure rapid recovery and reduce complications. Preventive strategies, particularly pneumococcal vaccination, have proven highly effective in decreasing disease incidence. Continued vigilance, combined with tailored treatment approaches and public health measures, is essential in managing this pervasive pediatric condition.