Pleural empyema, also referred to as empyema thoracis, is the accumulation of pus within the pleural cavity—the space between the lung and the chest wall—typically resulting from an infection such as pneumonia, lung abscess, or thoracic surgery. It is a severe condition that requires immediate medical attention to prevent life-threatening complications like sepsis, lung collapse, or fibrosis.
Anatomy of the Pleural Space and Pathogenesis of Empyema
The pleural cavity is a thin potential space lined by two layers: the visceral pleura covering the lungs and the parietal pleura lining the chest wall. Under normal conditions, it contains a minimal amount of lubricating fluid, facilitating lung expansion during respiration.
Pleural empyema occurs in three progressive stages:
- Exudative Phase: Thin, sterile fluid accumulates due to inflammation.
- Fibrinopurulent Phase: Bacterial invasion occurs, with thick pus formation and fibrin deposition causing loculations.
- Organizing Phase: Fibroblasts proliferate, creating a thick fibrous peel encasing the lung, often requiring surgical decortication.
Causes and Risk Factors of Pleural Empyema
Pleural empyema is typically secondary to an existing thoracic infection or trauma. Major causative agents include:
Infectious Sources
- Bacterial pneumonia (most common)
- Lung abscess rupture
- Tuberculosis
- Postoperative infections
- Esophageal perforation
Common Pathogens
- Streptococcus pneumoniae
- Staphylococcus aureus (including MRSA)
- Haemophilus influenzae
- Klebsiella pneumoniae
- Anaerobes and Gram-negative bacilli
Predisposing Conditions
- Immunosuppression
- Diabetes mellitus
- Chronic obstructive pulmonary disease (COPD)
- Alcoholism
- Thoracic trauma or surgical intervention
Clinical Features and Symptoms of Pleural Empyema
Symptoms of pleural empyema often mimic those of pneumonia but persist despite antibiotic treatment. Clinical signs include:
- Persistent fever and chills
- Pleuritic chest pain (worse with deep breaths)
- Cough with foul-smelling sputum
- Dyspnea or difficulty breathing
- Weight loss and fatigue
- Decreased breath sounds on auscultation
- Dullness to percussion on the affected side
Diagnostic Approach to Pleural Empyema
A prompt and accurate diagnosis is crucial to initiate targeted treatment and prevent complications. The diagnostic process involves:
Imaging Studies
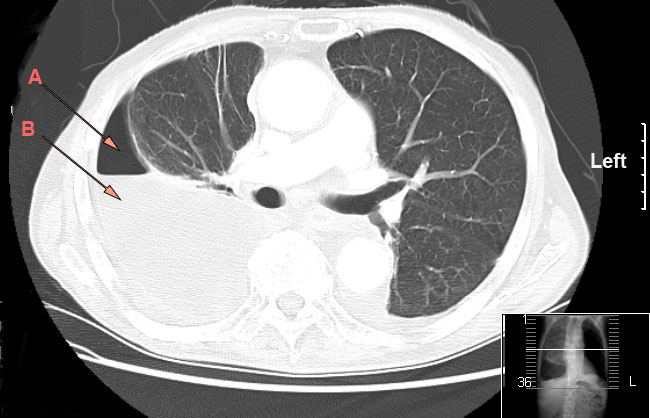
- Chest X-ray: Reveals pleural effusion or air-fluid levels.
- Ultrasound: Detects loculated fluid collections and guides thoracentesis.
- CT Scan: Provides detailed views of pleural thickening, loculations, and lung entrapment.
Thoracentesis and Pleural Fluid Analysis
Diagnostic thoracentesis confirms the presence of empyema by analyzing pleural fluid for:
- Appearance: Purulent or cloudy
- pH: < 7.2 suggests empyema
- Glucose: Low levels (< 40 mg/dL)
- LDH: Elevated (> 1000 IU/L)
- Gram stain and culture: Identify causative organisms
Management and Treatment of Pleural Empyema
Effective management of pleural empyema depends on the stage of disease progression and patient condition. The three pillars of treatment are antibiotics, drainage, and surgical intervention when required.
Antibiotic Therapy
Empirical broad-spectrum antibiotics are initiated based on local resistance patterns and later tailored according to culture results.
- Initial Regimens: β-lactam/β-lactamase inhibitor combinations, third-generation cephalosporins, or carbapenems
- Coverage: Gram-positive, Gram-negative, and anaerobic organisms
- Duration: Typically 3–6 weeks depending on response and resolution
Chest Tube Drainage
For fluid evacuation and infection control:
- Intercostal chest tube insertion under imaging guidance
- Fibrinolytics (e.g., tPA + DNase) to break loculations in the fibrinopurulent phase
- Continuous monitoring for output, resolution, and tube patency
Video-Assisted Thoracoscopic Surgery (VATS)
Minimally invasive approach for:
- Decortication of fibrinous peel
- Drainage of loculated pus
- Removal of necrotic tissue
VATS is preferred for patients with organized empyema not responding to chest tube drainage.
Open Thoracotomy and Decortication
Indicated in advanced-stage empyema where:
- Lung entrapment persists
- Extensive fibrous tissue hinders expansion
- VATS is insufficient or contraindicated
Prognosis and Potential Complications
Timely intervention significantly improves outcomes. However, if left untreated or mismanaged, pleural empyema can result in:
- Lung collapse
- Bronchopleural fistula
- Fibrothorax (permanent lung restriction)
- Sepsis and multiorgan failure
- Death in severe untreated cases
Preventive Measures for Pleural Empyema
Prompt Treatment of Pneumonia
Early administration of antibiotics in community- and hospital-acquired pneumonia reduces the risk of progression to empyema.
Vaccination
- Pneumococcal vaccine
- Haemophilus influenzae type B vaccine
- Influenza vaccine
These significantly reduce the incidence of primary infections that can lead to empyema.
Postoperative Care
Strict aseptic protocols and pulmonary rehabilitation post thoracic surgery reduce infection risk.
Pleural empyema is a life-threatening condition that arises from inadequate resolution of pleural infections. Early identification, appropriate imaging, microbiological analysis, and a tiered treatment strategy involving antibiotics, drainage, and surgery are essential to ensure full recovery. Multidisciplinary care, including pulmonology, infectious disease, and thoracic surgery teams, plays a vital role in effective management and long-term outcomes.