Plasmodium vivax, a protozoan parasite, presents unique challenges in malaria prevention due to its ability to form hypnozoites—dormant liver-stage parasites capable of causing relapses. These relapses can occur weeks or months after the initial infection, complicating control efforts and increasing the burden on endemic regions. Effective prevention requires integrated strategies targeting both the mosquito vector and the human host.
Lifecycle of Plasmodium Vivax and Points of Intervention
Understanding the lifecycle of P. vivax is essential to identify opportunities for effective prevention. The parasite alternates between mosquito and human hosts, with specific stages susceptible to intervention.
Vector Control: Breaking the Transmission Cycle
Insecticide-Treated Nets (ITNs)
Widespread distribution and use of ITNs remain the most cost-effective tool in preventing bites from Anopheles mosquitoes. These nets are treated with long-lasting insecticides, offering dual protection by creating both a physical and chemical barrier.
Indoor Residual Spraying (IRS)
IRS involves the application of insecticides on indoor walls where mosquitoes rest after feeding. Effective especially in high-transmission regions, IRS reduces mosquito lifespan and thus transmission potential.
Environmental Management
Reducing mosquito breeding grounds through improved drainage, proper waste disposal, and elimination of stagnant water is essential. Community-level engagement in habitat management can significantly lower vector density.
Personal Protection and Behavioral Interventions
Use of Repellents
Topical insect repellents containing DEET, picaridin, or oil of lemon eucalyptus are recommended, particularly during peak mosquito biting hours (dusk to dawn).
Protective Clothing
Wearing long-sleeved shirts, long pants, and closed shoes during outdoor activities in endemic regions reduces skin exposure and mosquito bites.
Housing Improvements
Structural modifications such as window screens, closed eaves, and ceiling fans can minimize indoor mosquito entry and reduce the risk of infection.
Chemoprophylaxis: Preventing Infection in High-Risk Groups
Chemoprophylaxis involves administering antimalarial drugs to prevent the establishment of infection in individuals exposed to malaria-endemic regions.
Primaquine for Terminal Prophylaxis
For travelers and military personnel returning from vivax-endemic areas, a 14-day course of primaquine is effective in preventing relapses. G6PD testing is mandatory due to the risk of hemolysis.
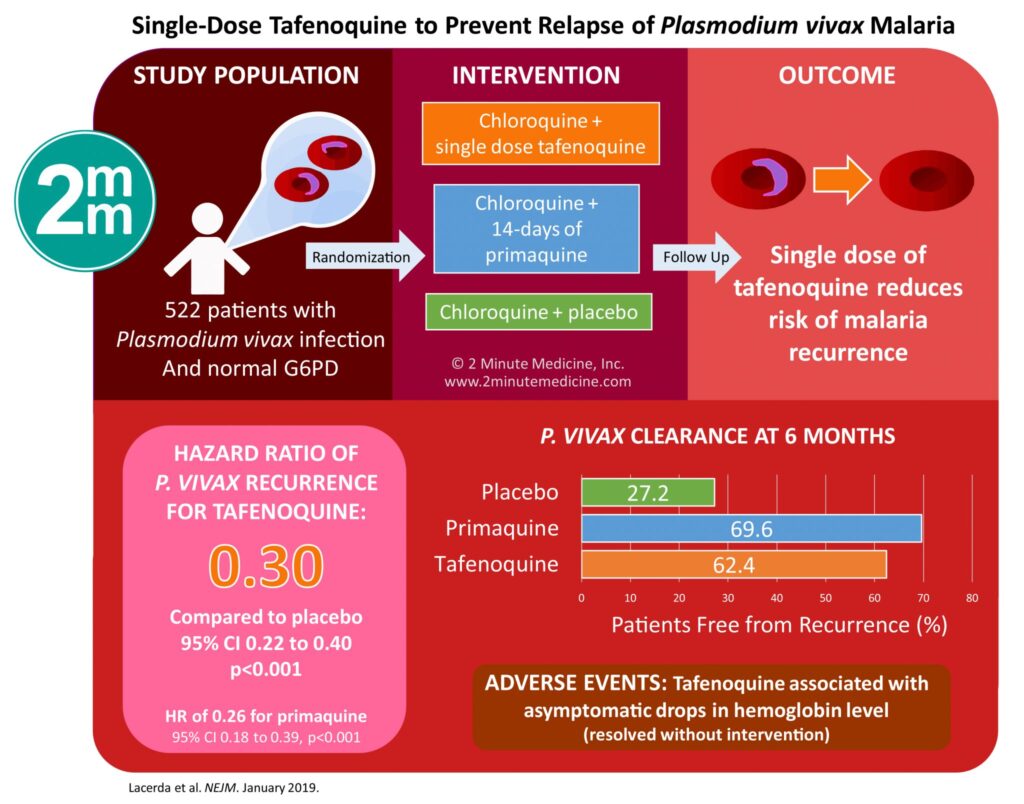
Tafenoquine: Single-Dose Alternative
Tafenoquine offers a single-dose alternative for radical cure and prophylaxis but also requires G6PD screening. It is a significant advancement in simplifying prevention strategies.
Chloroquine and Mefloquine
These agents are effective in suppressing blood-stage parasites but do not eliminate hypnozoites. They are suitable for short-term prophylaxis in regions with chloroquine-sensitive P. vivax.
Radical Cure: Eliminating Dormant Hypnozoites
Preventing relapses is central to P. vivax malaria control. Radical cure refers to treatment aimed at eradicating both blood-stage and liver-stage parasites.
Primaquine-Based Radical Cure
Primaquine is the only widely available hypnozoitocidal agent. Its efficacy in preventing relapses is well-established, provided the patient is G6PD-normal and adheres to the 14-day regimen.
Monitoring and Ensuring Adherence
Health systems must focus on patient education and adherence support, as incomplete treatment leads to persistent transmission and increased risk of resistance.
G6PD Deficiency Screening: A Prerequisite for Prevention
G6PD deficiency is a genetic disorder that increases vulnerability to hemolysis from drugs like primaquine and tafenoquine. Widespread implementation of point-of-care G6PD tests is vital to safely expand access to radical cure treatments.
Vaccine Development: A Promising Frontier
While no licensed vaccine currently targets Plasmodium vivax, several candidates are in clinical trials. Vaccine development focuses on targeting:
- Sporozoite antigens (preventing liver-stage infection)
- Merozoite surface proteins (blocking erythrocytic invasion)
- Transmission-blocking vaccines (reducing mosquito infectivity)
Progress in this field holds promise for long-term eradication strategies.
Surveillance and Community-Based Interventions
Active Case Detection
Active case detection through community screening and prompt treatment reduces the human reservoir and limits transmission.
Mass Drug Administration (MDA)
In high-transmission zones, MDA with antimalarials including primaquine or tafenoquine can reduce both symptomatic and asymptomatic infections.
Community Engagement and Health Education
Sustainable prevention relies on local involvement. Educational programs focused on recognizing symptoms, using protective tools, and seeking timely treatment are crucial.
Integration with National Malaria Elimination Programs
National and regional elimination programs must tailor prevention strategies to the unique biology of P. vivax. These programs should integrate:
- Vector control
- Prophylaxis
- Radical cure access
- Surveillance systems
- Research and policy support
Coordination among governments, NGOs, and health organizations is essential to reach elimination goals.
Preventing Plasmodium vivax malaria requires a multifaceted approach targeting both the mosquito vector and the parasite’s unique biology. From radical cure therapies and chemoprophylaxis to community education and vaccine research, a coordinated strategy is the cornerstone of effective control and eventual eradication. As relapsing infections continue to burden endemic communities, scaling up prevention efforts with precision, safety, and sustainability remains imperative.