Plasmodium vivax is one of the five protozoan species that cause malaria in humans. Unlike the often-deadly Plasmodium falciparum, P. vivax malaria is generally less severe but is notable for its ability to relapse due to dormant liver-stage parasites known as hypnozoites. Its widespread geographic distribution, especially across Asia and Latin America, makes it a major public health concern.
Morphology and Lifecycle of Plasmodium Vivax
P. vivax is a eukaryotic, unicellular organism belonging to the phylum Apicomplexa. Its lifecycle includes both human and mosquito hosts, with distinct hepatic and erythrocytic stages in humans and sexual reproduction in the Anopheles mosquito.
Key Lifecycle Features:
- Sporozoites: Infective form injected by mosquito.
- Hypnozoites: Dormant liver-stage forms responsible for relapse.
- Merozoites: Invade red blood cells, initiating the symptomatic phase.
- Gametocytes: Sexual stage ingested by mosquitoes.
Geographical Distribution and Epidemiology
P. vivax malaria is endemic in:
- South and Southeast Asia
- Latin America
- Parts of the Middle East and Oceania
It is less prevalent in sub-Saharan Africa due to the high frequency of Duffy-negative individuals, who are resistant to P. vivax infection due to the absence of Duffy antigens on red blood cells.
Clinical Manifestations and Symptoms
Symptoms typically emerge 10–17 days post-infection and coincide with the rupture of infected erythrocytes. The hallmark features of P. vivax malaria include:
- Cyclic fevers (every 48 hours – tertian malaria)
- Chills and rigors
- Sweating
- Headache
- Nausea and vomiting
- Splenomegaly
- Fatigue and anemia
Relapses can occur weeks or months after initial infection due to reactivation of hypnozoites.
Diagnosis of Plasmodium Vivax Malaria
Accurate diagnosis is essential for effective treatment. Diagnostic methods include:
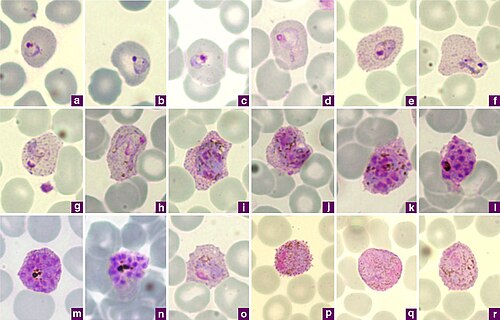
1. Microscopy
- Gold standard.
- Detection of trophozoites and schizonts in Giemsa-stained blood films.
2. Rapid Diagnostic Tests (RDTs)
- Detect P. vivax–specific antigens (e.g., PvLDH).
- Useful in remote or resource-limited settings.
3. Polymerase Chain Reaction (PCR)
- High sensitivity and specificity.
- Used in epidemiological studies and cases with low parasitemia.
Treatment Strategies for Plasmodium Vivax
1. Acute Blood-Stage Treatment
- Chloroquine: First-line treatment in regions without resistance.
- Artemisinin-based Combination Therapies (ACTs): Used where resistance is suspected.
2. Radical Cure
- Targets hypnozoites to prevent relapse.
- Primaquine: 14-day course; requires G6PD deficiency screening.
- Tafenoquine: Single-dose alternative; also requires G6PD testing.
3. Management of Complications
- Supportive care for anemia, dehydration, and in rare cases, severe malaria.
Relapse and Hypnozoite Activation
The defining characteristic of P. vivax is its ability to cause relapse. Hypnozoites can remain dormant for weeks or months. Factors influencing relapse include:
- Host immune status
- Geographical strain differences
- Inadequate radical cure
Managing relapses is vital for individual health and community transmission control.
Prevention and Control Measures
1. Vector Control
- Insecticide-treated bed nets (ITNs)
- Indoor residual spraying (IRS)
- Larval source management
2. Chemoprophylaxis
- For travelers to endemic regions.
- Primaquine-based prophylaxis, subject to G6PD status.
3. Surveillance and Elimination Programs
- Active case detection
- Mass drug administration in high-burden zones
- Integration with national malaria elimination frameworks
Challenges and Emerging Concerns
- Drug resistance: Chloroquine resistance in parts of Southeast Asia.
- G6PD deficiency: Limits use of hypnozoitocidal drugs in certain populations.
- Asymptomatic carriers: Maintain transmission reservoirs.
- Diagnostic limitations: RDTs may miss low-density infections.
Future Outlook and Research Directions
- New drug development: Safer hypnozoitocidal agents.
- Vaccine research: Targeting sporozoite and liver stages.
- Genomic studies: Understanding parasite diversity and drug resistance.
Plasmodium vivax malaria remains a formidable challenge due to its relapsing nature, widespread distribution, and growing drug resistance. A multi-pronged approach combining effective diagnosis, treatment, prevention, and global research collaboration is crucial to achieving control and eventual elimination.