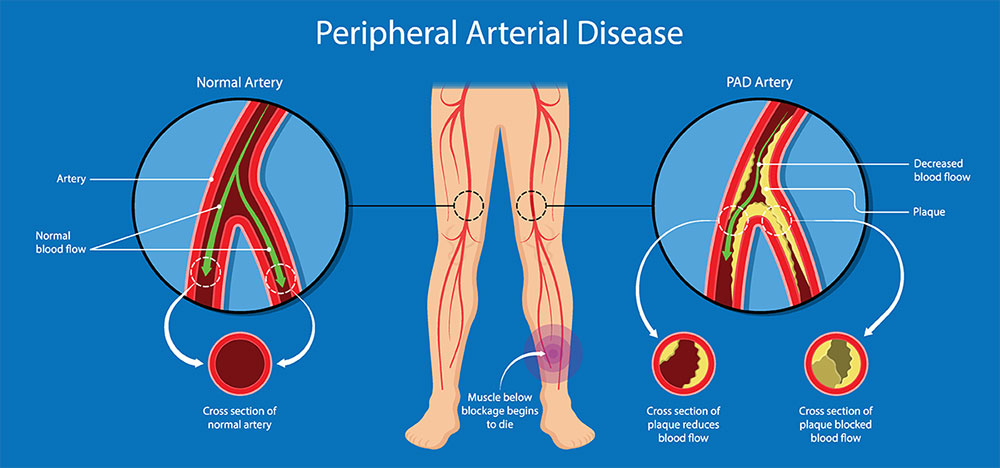
Peripheral Vascular Disease (PVD), also referred to as Peripheral Artery Disease (PAD), is a circulatory disorder that affects the blood vessels outside the heart and brain, most commonly in the legs and arms. It leads to narrowed or blocked arteries, reducing blood flow and resulting in significant health complications if left untreated.
What Is Peripheral Vascular Disease?
Peripheral Vascular Disease is primarily caused by atherosclerosis, a condition in which fatty deposits accumulate in the arterial walls, leading to reduced blood circulation. PVD can affect both arteries (arterial disease) and veins (venous disease), but it is most commonly associated with arterial involvement in the lower extremities.
Key Symptoms of Peripheral Vascular Disease
Recognizing the early signs of PVD can prevent serious complications. Common symptoms include:
- Claudication: Cramping or pain in the legs during physical activity, relieved by rest.
- Numbness or weakness in the limbs
- Coldness in lower legs or feet, especially when compared to the other limb
- Sores or wounds on toes, feet, or legs that do not heal
- Color changes in the skin of the legs
- Hair loss or slower hair growth on legs and feet
- Shiny skin on the legs
- Weak or absent pulse in legs or feet
In severe cases, critical limb ischemia may occur, which can lead to tissue death and possible amputation.
Primary Causes and Risk Factors
The most common cause of PVD is atherosclerosis, but several other factors contribute to the onset and progression of the disease:
Major Risk Factors:
- Smoking: The single most important modifiable risk factor
- Diabetes: Increases risk of arterial damage
- High blood pressure and cholesterol
- Obesity and sedentary lifestyle
- Age over 50
- Family history of cardiovascular disease
- Chronic kidney disease
Types of Peripheral Vascular Disease
PVD is broadly categorized into:
1. Functional PVD
This type does not involve physical damage to blood vessels. Spasms in the vessels cause temporary narrowing. Common conditions include Raynaud’s disease.
2. Organic PVD
This involves structural changes in the blood vessels due to inflammation, plaque, or damage. Atherosclerosis is the leading cause.
How Peripheral Vascular Disease Is Diagnosed
Early diagnosis is crucial. Diagnostic procedures may include:
- Ankle-Brachial Index (ABI): Compares blood pressure in the ankle and arm
- Doppler Ultrasound: Measures blood flow through arteries and veins
- Angiography: Uses X-ray imaging to visualize blood vessels after dye injection
- Magnetic Resonance Angiography (MRA) or CT Angiography
- Blood Tests: Assess cholesterol, blood sugar, and inflammatory markers
Treatment Options for Peripheral Vascular Disease
1. Lifestyle Modifications
- Quit smoking
- Adopt a healthy diet (low in saturated fats and sugars)
- Regular physical activity, such as supervised walking programs
- Weight loss
2. Medications
- Antiplatelet agents (e.g., aspirin, clopidogrel)
- Cholesterol-lowering drugs (statins)
- Blood pressure medications
- Cilostazol or pentoxifylline for improving walking distance
3. Minimally Invasive Procedures
- Angioplasty: Inflates a balloon to open up narrowed arteries
- Stent placement: Keeps the artery open after angioplasty
- Atherectomy: Removal of plaque from the artery
4. Surgical Interventions
- Bypass surgery: Creates a detour around blocked arteries using a graft
Preventing Peripheral Vascular Disease
Preventive strategies significantly lower the risk:
- Maintain optimal blood pressure and glucose levels
- Engage in regular cardiovascular exercise
- Eat a heart-healthy diet rich in fruits, vegetables, and whole grains
- Refrain from tobacco use
- Attend regular screenings, especially if at risk
Complications of Untreated Peripheral Vascular Disease
Ignoring symptoms or delaying treatment can result in:
- Critical limb ischemia
- Infection and gangrene
- Increased risk of heart attack and stroke
- Amputation of affected limb
Living With Peripheral Vascular Disease
Effective management of PVD requires lifelong commitment. Patients should:
- Monitor cardiovascular health regularly
- Adhere strictly to treatment plans
- Participate in rehabilitation programs
- Communicate with healthcare providers regarding symptom progression
Frequently Asked Questions:
What is the difference between PAD and PVD?
Peripheral Artery Disease (PAD) is a subset of Peripheral Vascular Disease (PVD) that specifically involves narrowing of arteries, while PVD may include venous disorders as well.
Can Peripheral Vascular Disease be reversed?
While PVD cannot be completely reversed, its progression can be slowed, and symptoms managed effectively through lifestyle changes, medications, and procedures.
Is walking good for PVD?
Yes. Supervised walking therapy improves circulation, reduces symptoms, and enhances mobility.
How serious is Peripheral Vascular Disease?
If left untreated, PVD can lead to life-threatening complications such as limb amputation, stroke, or heart attack.
What are the early warning signs of PVD?
Leg pain during walking, cold feet, slow-healing wounds, and shiny skin on legs are among the earliest symptoms.
Peripheral Vascular Disease is a serious yet manageable condition. Early diagnosis, lifestyle changes, and proper medical interventions can dramatically improve outcomes. Individuals at risk or experiencing symptoms should seek timely evaluation to prevent complications and ensure long-term vascular health.