Peripheral arterial thromboembolism is a critical vascular condition resulting from the obstruction of peripheral arteries by embolic material, often originating from the heart or proximal arterial segments. These emboli can rapidly occlude blood flow to distal limbs, leading to acute limb ischemia, tissue necrosis, or amputation if not promptly managed.
Effective prevention is paramount to reduce morbidity, mortality, and recurrence. A multifaceted approach encompassing pharmacologic therapy, risk factor modification, and vigilant clinical surveillance is essential.
Pathogenesis of Thromboembolic Events in Peripheral Arteries
Emboli typically consist of thrombotic material, cholesterol crystals, or cardiac vegetations. The most common sources include:
- Atrial fibrillation – leading to thrombus formation in the left atrial appendage.
- Left ventricular mural thrombi – often post-myocardial infarction.
- Prosthetic heart valves – due to altered flow dynamics.
- Atherosclerotic plaque rupture – with embolization of debris.
These emboli travel distally and lodge in narrow arterial branches, leading to a sudden interruption in blood supply.
Identifying High-Risk Patients
The likelihood of peripheral arterial thromboembolism increases in individuals with the following risk profiles:
- Cardiac arrhythmias – especially atrial fibrillation or flutter.
- Structural heart disease – including valvular heart defects or cardiomyopathy.
- Post-surgical status – following vascular or orthopedic interventions.
- Known peripheral artery disease (PAD) – increases baseline vascular risk.
- Hypercoagulable states – genetic or acquired thrombophilia.
Patients over 65 years of age or with a history of embolic events are particularly vulnerable and require aggressive preventive strategies.
Clinical Consequences of Thromboembolic Events
Peripheral arterial thromboembolism can present abruptly with the following symptoms:
- Sudden limb pain
- Pallor and pulselessness
- Cold extremities
- Motor or sensory loss
- Possible cyanosis or mottling
If untreated, this may progress to irreversible ischemia, muscle necrosis, infection, or limb loss within hours. Prompt recognition and urgent intervention are crucial.
Diagnostic Evaluation for Thromboembolic Risk
Thorough diagnostics allow for both immediate intervention and long-term prevention. The following tools are recommended:
Non-Invasive Diagnostics:
- Ankle-Brachial Index (ABI) – Identifies underlying PAD.
- Duplex Ultrasonography – Detects embolus location and assesses blood flow.
- Echocardiography – Identifies cardiac sources such as thrombi or valvular disease.
- Electrocardiogram (ECG) – Confirms arrhythmias like atrial fibrillation.
Advanced Imaging:
- CT Angiography (CTA) – Offers high-resolution imaging of arterial blockages.
- MR Angiography (MRA) – Suitable for patients with renal impairment or contrast allergies.
Evidence-Based Strategies for Peripheral Arterial Thromboembolism Prevention
1. Antithrombotic and Anticoagulant Therapy
Antithrombotic therapy forms the cornerstone of embolism prevention.
Antiplatelet Agents:
- Aspirin – Reduces platelet aggregation.
- Clopidogrel – Used in aspirin-intolerant patients or dual antiplatelet therapy (DAPT) settings.
Anticoagulants:
- Warfarin – Indicated for atrial fibrillation and mechanical valves; requires INR monitoring.
- Direct Oral Anticoagulants (DOACs) – Such as apixaban, rivaroxaban; offer fixed dosing with fewer monitoring requirements.
Selection depends on the underlying pathology and risk stratification.
2. Management of Cardiac Conditions
Effective control of cardiac conditions is critical:
- Rhythm control in atrial fibrillation
- Valve repair/replacement when indicated
- Left atrial appendage occlusion in non-valvular AF patients intolerant to anticoagulation
3. Atherosclerosis Control and Risk Factor Modification
- Smoking cessation – Immediate and profound risk reduction.
- Lipid-lowering therapy – Statins to achieve LDL <70 mg/dL in high-risk patients.
- Hypertension control – Target <130/80 mmHg.
- Diabetes management – Maintain HbA1c <7%.
- Weight optimization and regular exercise – Improve vascular function and insulin sensitivity.
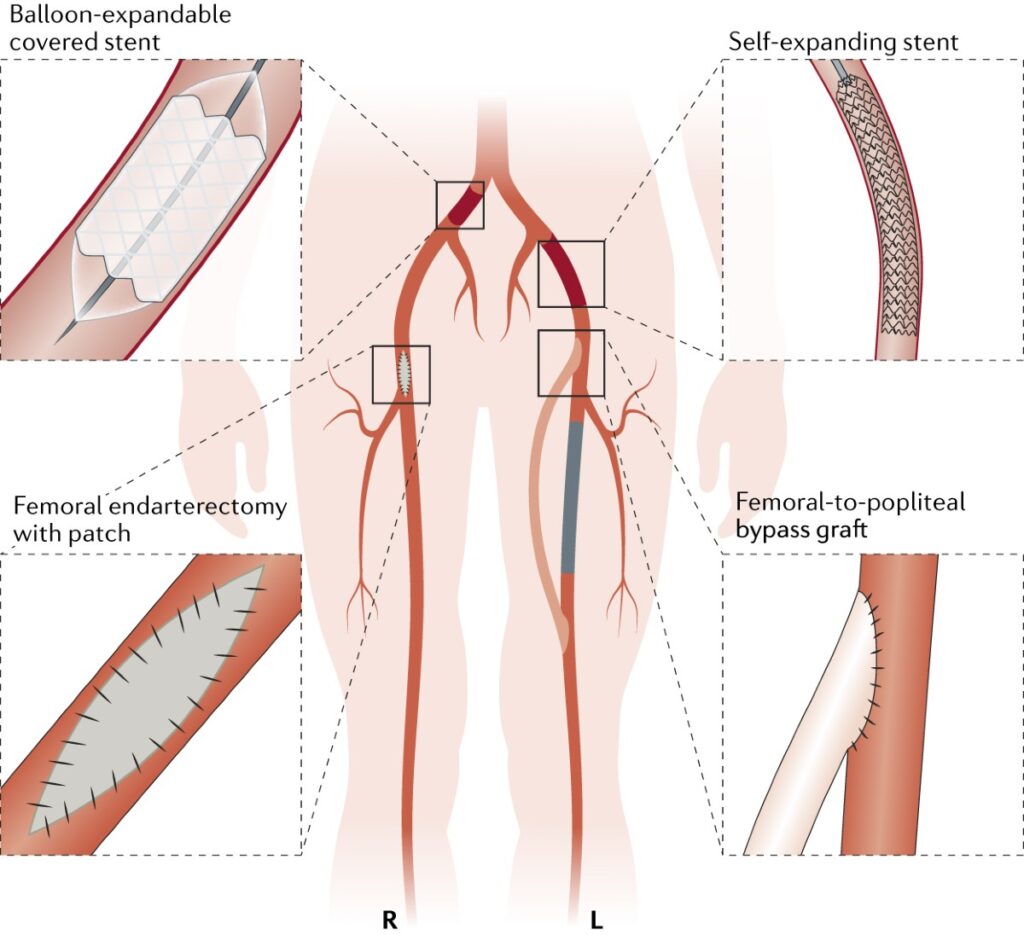
4. Surgical and Endovascular Interventions
Preventive interventions may include:
- Endarterectomy – Removes atherosclerotic plaques from arteries.
- Bypass grafting – In cases of severe PAD to maintain perfusion.
- Embolectomy – Urgent removal of emboli in acute events.
Such procedures are reserved for high-risk or recurrent patients with failed medical therapy.
Monitoring and Long-Term Follow-Up
Long-term care is vital for sustained prevention:
- Regular duplex scans to monitor arterial patency.
- ECG and echocardiography reviews for cardiac source detection.
- Therapeutic drug monitoring in patients on warfarin.
- Adherence checks for antiplatelet and anticoagulant therapies.
Annual follow-ups, lifestyle reinforcement, and medication review reduce recurrence and improve prognosis.
Peripheral arterial thromboembolism poses a significant risk to limb viability and patient survival. A proactive and comprehensive preventive strategy—focusing on anticoagulation, cardiac care, lifestyle modification, and regular monitoring—is essential for mitigating this threat. By identifying high-risk patients early and implementing personalized interventions, we can significantly reduce the incidence and severity of thromboembolic events, preserving both limb and life.