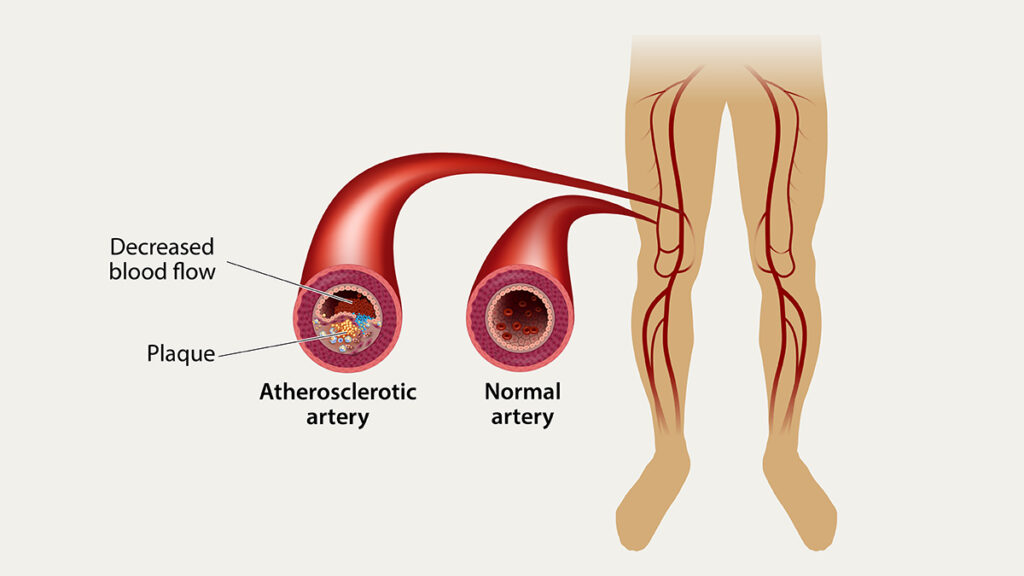
Peripheral arterial occlusive disease (PAOD), also referred to as peripheral artery disease (PAD), is a chronic circulatory condition characterized by narrowed arteries that reduce blood flow to the limbs, most commonly the legs. PAOD is a manifestation of systemic atherosclerosis, often affecting the lower extremities due to plaque buildup in peripheral arteries. This results in diminished oxygen supply to the muscles and tissues, leading to pain, impaired mobility, and in advanced cases, tissue loss.
Pathophysiology: How Atherosclerosis Leads to Arterial Blockage
Atherosclerosis is the primary mechanism underlying PAOD. It involves the progressive accumulation of lipids, cholesterol, calcium, and cellular debris within the arterial wall, forming atheromatous plaques. These plaques cause the arterial lumen to narrow and harden, impeding blood flow and oxygen delivery to peripheral tissues.
Key Risk Factors Associated with PAOD
Multiple risk factors contribute to the development and progression of PAOD. These include:
- Smoking – A significant independent risk factor, accelerating arterial damage.
- Diabetes Mellitus – Promotes atherosclerosis and microvascular complications.
- Hypertension – Increases arterial wall stress, fostering plaque formation.
- Hyperlipidemia – Elevated LDL cholesterol contributes to plaque development.
- Advanced Age – Risk increases significantly after age 50.
- Sedentary Lifestyle – Physical inactivity reduces collateral circulation.
- Family History of Cardiovascular Disease – Indicates genetic predisposition.
Clinical Manifestations: Symptoms and Stages of PAOD
The clinical presentation of PAOD varies by severity, classified into stages by the Fontaine or Rutherford systems. Symptoms range from asymptomatic to severe limb-threatening ischemia.
Common Symptoms:
- Intermittent Claudication – Cramping pain in calves or thighs during walking, relieved by rest.
- Rest Pain – Pain in the foot at rest, often at night.
- Cold or Numb Limbs – Due to inadequate blood flow.
- Non-Healing Ulcers – Typically on toes, heels, or pressure points.
- Gangrene – Tissue death due to prolonged ischemia.
Fontaine Classification:
- Stage I: Asymptomatic
- Stage II: Intermittent claudication
- IIa: Walking distance >200 meters
- IIb: Walking distance <200 meters
- Stage III: Ischemic rest pain
- Stage IV: Ulceration or gangrene
Diagnostic Approach: Confirming Peripheral Arterial Occlusive Disease
Early and accurate diagnosis is essential to prevent complications. We use a combination of clinical evaluation and diagnostic tools.
Ankle-Brachial Index (ABI)
- ABI < 0.90 confirms PAOD.
- A simple, non-invasive test comparing blood pressure in the ankle to the arm.
Additional Diagnostic Tests:
- Doppler Ultrasound – Assesses blood flow velocity and detects occlusions.
- CTA (Computed Tomography Angiography) – Provides detailed imaging of arterial structures.
- MRA (Magnetic Resonance Angiography) – An alternative for patients with renal insufficiency.
- Conventional Angiography – Gold standard for identifying lesion morphology before revascularization.
Management and Treatment Options for PAOD
Treatment aims to relieve symptoms, improve quality of life, and prevent limb loss or cardiovascular events. Management includes lifestyle modification, pharmacotherapy, and revascularization.
Lifestyle and Risk Factor Modification
- Smoking cessation – Absolute priority.
- Exercise therapy – Supervised walking programs enhance collateral circulation.
- Dietary changes – Low-saturated fat, high-fiber diets improve lipid profiles.
- Glycemic control – Essential for diabetic patients.
Pharmacologic Therapy
- Antiplatelet agents (aspirin or clopidogrel) – Reduce risk of thrombosis.
- Statins – Lower cholesterol and stabilize plaque.
- Cilostazol – Improves walking distance in claudication.
- ACE inhibitors – Cardiovascular risk reduction.
Revascularization Procedures
Revascularization is considered in severe cases or when conservative management fails.
Endovascular Interventions
- Angioplasty with or without Stenting – Minimally invasive; used for short segment stenoses.
- Atherectomy – Removal of atherosclerotic plaque using specialized devices.
Surgical Interventions
- Bypass Grafting – Creation of an alternative blood flow route using synthetic or autologous grafts.
- Endarterectomy – Surgical removal of plaque from the artery.
Complications of Untreated PAOD
If left untreated, PAOD can progress to critical limb ischemia (CLI), characterized by persistent rest pain, ulcers, and gangrene, often resulting in:
- Limb amputation
- Severe infection
- Disability
- Increased cardiovascular mortality
Preventive Measures and Long-Term Monitoring
Preventing progression and complications requires continuous management.
- Regular ABI screening in at-risk populations.
- Long-term antiplatelet therapy to reduce ischemic events.
- Annual foot exams for diabetics with PAOD.
- Close monitoring of lipid levels and blood pressure.
Peripheral arterial occlusive disease is a serious yet manageable condition when detected early. Comprehensive risk factor control, lifestyle intervention, and appropriate medical or surgical treatment are essential in reducing morbidity, improving limb salvage, and enhancing patient outcomes. Prompt recognition of symptoms, coupled with accurate diagnosis and targeted treatment, remains the cornerstone of successful management.