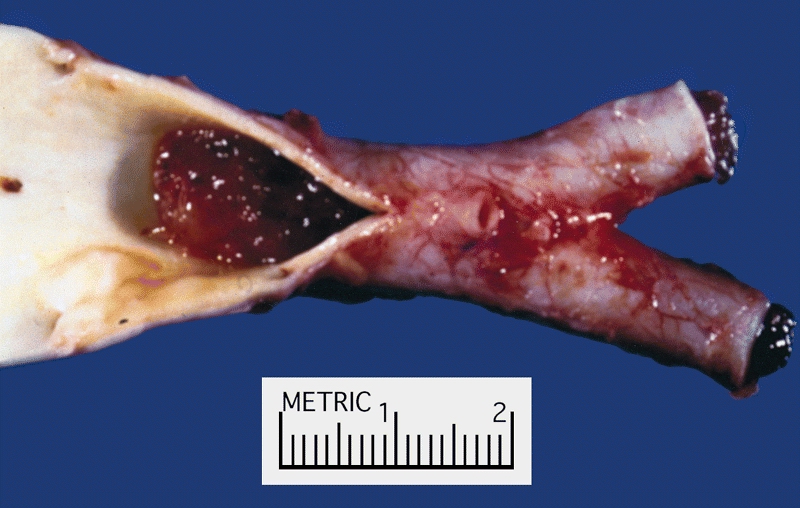
Peripheral arterial embolism (PAE) is a sudden blockage of an artery in the limbs due to an embolus—commonly a blood clot—that travels through the bloodstream and lodges in a peripheral artery. This condition leads to acute limb ischemia, a vascular emergency requiring prompt diagnosis and intervention to prevent permanent tissue damage or limb loss.
Pathophysiology of Peripheral Arterial Embolism
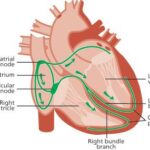
An embolus is a detached intravascular mass that travels through the bloodstream and causes blockage in a distant vessel. In PAE, emboli typically originate from the heart, especially in conditions like atrial fibrillation, myocardial infarction, or valvular heart disease. Once lodged in a peripheral artery, the embolus obstructs blood flow, leading to ischemia and potential infarction of the affected tissues.
Etiology and Risk Factors
The primary sources of emboli causing PAE include:
- Cardiac sources: Atrial fibrillation, myocardial infarction, prosthetic heart valves, and infective endocarditis.
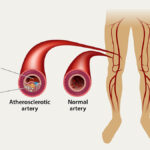
- Aortic sources: Atheromatous plaques or aneurysms.
- Paradoxical embolism: Emboli originating from the venous system crossing into arterial circulation through a patent foramen ovale.
Risk factors encompass:
- Advanced age
- Smoking
- Hypertension
- Diabetes mellitus
- Hyperlipidemia
- Previous history of embolic events
Clinical Presentation
The hallmark of PAE is the sudden onset of symptoms in the affected limb, often described by the “6 Ps”:
- Pain: Severe and sudden in onset.
- Pallor: Pale appearance of the limb.
- Pulselessness: Absence of distal pulses.
- Paresthesia: Numbness or tingling sensations.
- Paralysis: Loss of motor function.
- Poikilothermia: Coolness of the limb.
Prompt recognition of these signs is crucial for timely intervention.
Diagnostic Evaluation
A thorough clinical assessment is the first step, followed by diagnostic imaging to confirm the diagnosis and plan treatment.
Imaging Modalities
- Doppler Ultrasound: Non-invasive and useful for assessing blood flow and locating occlusions.
- Computed Tomography Angiography (CTA): Provides detailed images of blood vessels, aiding in precise localization of the embolus.
- Magnetic Resonance Angiography (MRA): An alternative to CTA, especially in patients with contraindications to iodinated contrast.
Treatment Strategies
The primary goal in managing PAE is to restore blood flow promptly to prevent tissue necrosis. Treatment options include:
Medical Management
- Anticoagulation: Immediate initiation of heparin to prevent further clot propagation.
Surgical Intervention
- Embolectomy: Surgical removal of the embolus, often using a Fogarty catheter.
- Bypass Surgery: Creating an alternative pathway for blood flow around the blockage.
Endovascular Techniques
- Catheter-Directed Thrombolysis: Delivery of thrombolytic agents directly to the site of the embolus.
- Percutaneous Mechanical Thrombectomy: Minimally invasive removal of the embolus using specialized devices.
Prognosis and Complications
The prognosis of PAE largely depends on the timeliness of intervention. Delayed treatment can lead to:
- Permanent limb damage
- Amputation
- Systemic complications such as kidney failure or stroke
Early diagnosis and prompt revascularization are critical to improving outcomes.
Prevention
Preventive measures focus on managing risk factors and underlying conditions:
- Anticoagulation Therapy: For patients with atrial fibrillation or other cardiac conditions prone to emboli formation.
- Lifestyle Modifications: Smoking cessation, regular exercise, and dietary changes.
- Regular Monitoring: Routine check-ups for patients with known cardiovascular diseases.
Peripheral arterial embolism is a vascular emergency that necessitates immediate medical attention. Understanding its etiology, recognizing early symptoms, and initiating prompt treatment are paramount in preventing severe complications and improving patient outcomes.