Perennial allergic rhinitis is a chronic inflammatory condition of the nasal passages, triggered by allergens that persist throughout the year. Unlike seasonal allergic rhinitis, which is typically caused by pollen and other outdoor allergens, perennial allergic rhinitis is most often induced by indoor allergens such as dust mites, mold spores, pet dander, and cockroach droppings. It significantly impairs quality of life, leading to sleep disturbances, fatigue, and persistent nasal symptoms.
Pathophysiology of Perennial Allergic Rhinitis
The immunological response underlying perennial allergic rhinitis is an IgE-mediated hypersensitivity reaction. Upon exposure to specific allergens, sensitized individuals experience an immediate release of histamine, leukotrienes, and other inflammatory mediators from mast cells and basophils. This triggers vasodilation, mucosal edema, increased mucus secretion, and infiltration of eosinophils and T-helper 2 (Th2) lymphocytes.
Common Indoor Allergens in Perennial Allergic Rhinitis
Dust Mites
Dust mites thrive in warm, humid environments such as bedding, upholstered furniture, and carpets. Their fecal particles and body fragments are potent allergens.
Pet Dander
Proteins found in the saliva, skin flakes, and urine of cats and dogs can trigger persistent nasal inflammation in sensitized individuals.
Mold Spores
Indoor molds proliferate in damp, poorly ventilated spaces like bathrooms, basements, and kitchens. Airborne spores can be inhaled year-round.
Cockroach Allergen
Cockroach feces, saliva, and body parts contribute to allergic reactions, particularly in densely populated urban environments.
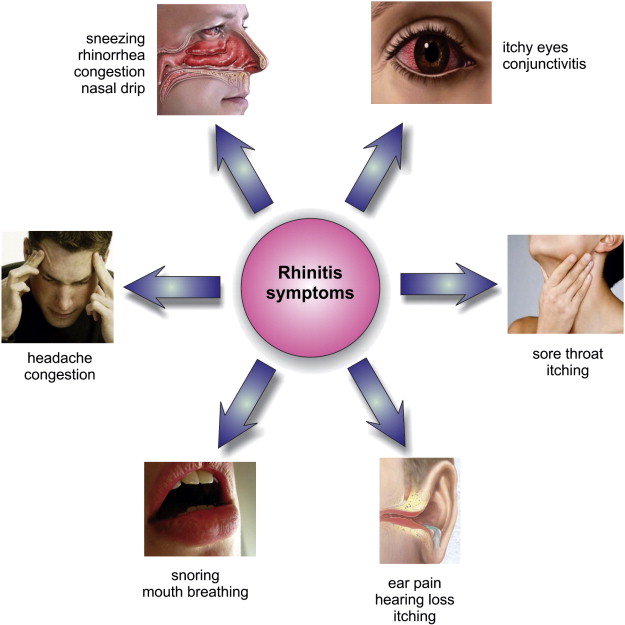
Symptoms of Perennial Allergic Rhinitis
The clinical presentation of perennial allergic rhinitis includes:
- Persistent nasal congestion
- Rhinorrhea (runny nose)
- Sneezing episodes
- Nasal itching
- Postnasal drip
- Decreased sense of smell
- Headaches due to sinus pressure
- Fatigue and irritability
- Sleep disturbances, especially due to nocturnal symptoms
Unlike seasonal allergic rhinitis, these symptoms occur throughout the year, often worsening in indoor environments.
Diagnostic Evaluation
Clinical History and Physical Examination
Diagnosis begins with a thorough clinical history focusing on the chronicity of symptoms, family history of atopy, environmental exposures, and response to previous treatments.
Skin Prick Testing
A widely used method to identify allergen sensitivities. Small amounts of common allergens are introduced into the skin to monitor for localized reactions.
Serum Specific IgE Testing
Blood tests can detect circulating IgE antibodies against specific allergens, useful when skin testing is contraindicated.
Nasal Endoscopy and Imaging
In patients with atypical or refractory symptoms, nasal endoscopy or sinus imaging (CT scan) can help rule out structural abnormalities or chronic sinusitis.
Evidence-Based Treatment Options
Allergen Avoidance
Although complete elimination is often impractical, reducing exposure to known triggers is foundational in managing perennial allergic rhinitis.
| Allergen Type | Recommended Control Measures |
|---|---|
| Dust Mites | Use hypoallergenic bedding, wash sheets weekly at ≥60°C, dehumidify indoor air |
| Pet Dander | Keep pets out of bedrooms, frequent grooming, HEPA air filtration |
| Mold | Fix leaks, improve ventilation, use dehumidifiers, clean with antifungal agents |
| Cockroaches | Maintain cleanliness, seal food, use insect traps and professional pest control |
Pharmacological Therapy
Intranasal Corticosteroids
First-line therapy due to potent anti-inflammatory effects. Examples include fluticasone, budesonide, and mometasone.
Oral and Intranasal Antihistamines
Second-generation antihistamines like cetirizine, loratadine, and fexofenadine are preferred for their non-sedative profile.
Leukotriene Receptor Antagonists
Montelukast can be beneficial, especially in patients with concurrent asthma.
Decongestants
Short-term use of intranasal decongestants (oxymetazoline) may offer symptomatic relief, but prolonged use leads to rhinitis medicamentosa.
Saline Nasal Irrigation
Improves mucociliary clearance and reduces mucosal inflammation when used regularly.
Immunotherapy: Long-Term Desensitization
Allergen-specific immunotherapy, administered either subcutaneously (SCIT) or sublingually (SLIT), modifies the underlying allergic response.
Benefits
- Reduces symptom severity and medication use
- Provides long-term disease modification
- May prevent the progression to asthma
Indications
- Inadequate symptom control with pharmacotherapy
- Desire to reduce long-term medication use
- Sensitization to unavoidable allergens
Pediatric and Geriatric Considerations
Children
Early identification and management are crucial to prevent complications such as otitis media, sinusitis, and impaired school performance. Growth monitoring is essential when using corticosteroids.
Elderly
Polypharmacy, cognitive decline, and coexisting cardiovascular conditions necessitate cautious use of systemic antihistamines and decongestants.
Impact on Quality of Life and Comorbidities
Perennial allergic rhinitis contributes to:
- Decreased cognitive performance
- Daytime fatigue and sleep disorders
- Worsening of comorbid conditions like asthma, sinusitis, and otitis media
- Increased healthcare utilization and work absenteeism
Emerging Therapies and Research Directions
Biologic Agents
Monoclonal antibodies such as omalizumab (anti-IgE) show promise in refractory allergic rhinitis, particularly with comorbid asthma.
Novel Intranasal Formulations
Combination sprays containing antihistamines and corticosteroids (e.g., azelastine-fluticasone) offer superior efficacy.
Gene-Environment Interaction Studies
Research into epigenetics and environmental modifiers aims to personalize treatment strategies based on genetic predisposition.
Prevention Strategies and Public Health Recommendations
- Promote awareness of indoor allergens
- Improve housing conditions, particularly in urban and low-income areas
- Advocate for early diagnosis and appropriate treatment to mitigate disease progression
Frequently Asked Questions
Q1. Can perennial allergic rhinitis be cured?
While there is no definitive cure, symptoms can be effectively managed with avoidance, medications, and immunotherapy.
Q2. Is immunotherapy safe for children?
Yes, both SCIT and SLIT are safe and effective in pediatric populations when administered under medical supervision.
Q3. How can I tell if my allergies are perennial or seasonal?
Perennial allergies occur year-round, often worsening indoors, whereas seasonal allergies are linked to outdoor pollen exposure and follow a seasonal pattern.
Q4. Are intranasal steroids safe for long-term use?
Yes, when used correctly, intranasal corticosteroids are safe and effective with minimal systemic absorption.
Q5. What’s the difference between perennial allergic rhinitis and non-allergic rhinitis?
Perennial allergic rhinitis is IgE-mediated and allergen-specific, while non-allergic rhinitis is triggered by irritants like smoke, weather, or strong odors without an allergic basis.

