A tubo-ovarian abscess (TOA) represents a severe complication of pelvic inflammatory disease (PID), involving the fallopian tube, ovary, and often adjacent pelvic structures. Peptostreptococcus spp., a group of anaerobic, gram-positive cocci, are key pathogens in the development of this condition due to their ability to thrive in necrotic, poorly oxygenated environments. These organisms are part of the endogenous vaginal flora but become pathogenic when ascending infection breaches normal anatomical barriers.
Pathophysiology of Peptostreptococcus-Induced TOA
The pathogenesis of Peptostreptococcus tubo-ovarian abscess begins with microbial ascent from the lower genital tract. In the context of PID, disrupted mucosal defenses facilitate colonization of the upper reproductive tract. Peptostreptococcus, often in synergy with other anaerobes and facultative organisms, induces inflammation, pus formation, and encapsulation of infected adnexal tissues.
Microbiology and Co-pathogens in TOA
Peptostreptococcus rarely acts alone. TOA is characteristically polymicrobial, involving both anaerobic and facultative bacteria. The presence of Peptostreptococcus spp. enhances the pathogenic synergy, as their metabolic byproducts support cohabitating organisms.
Common Co-Isolated Microorganisms
- Bacteroides fragilis
- Prevotella spp.
- Fusobacterium spp.
- Escherichia coli
- Streptococcus agalactiae
- Gardnerella vaginalis
This microbial diversity complicates treatment, often necessitating broad-spectrum antibiotics.
Clinical Presentation and Diagnostic Indicators
TOA caused by Peptostreptococcus typically presents insidiously, progressing to severe illness if untreated. Symptoms may mimic other gynecologic or gastrointestinal disorders.
Symptoms
- Persistent lower abdominal or pelvic pain
- Fever and chills
- Nausea or vomiting
- Vaginal discharge, often foul-smelling
- Painful intercourse (dyspareunia)
- Irregular menstrual bleeding
- Palpable adnexal mass on examination
Diagnostic Evaluation
- Pelvic ultrasound: First-line imaging; reveals complex, multiloculated adnexal mass
- CT/MRI scan: Confirms extent of disease or complications
- CBC: Elevated white blood cell count
- CRP/ESR: Raised inflammatory markers
- Endocervical/vaginal swabs: Culture and PCR to identify anaerobic pathogens
- Blood cultures: Indicated in systemic infection or septic presentation
Risk Factors and Predisposing Conditions
The development of a Peptostreptococcus-associated tubo-ovarian abscess is strongly associated with factors that predispose to upper genital tract infections.
Risk Factors
- Untreated or recurrent pelvic inflammatory disease
- Intrauterine device (IUD) use
- Recent gynecologic procedures (e.g., endometrial biopsy, hysteroscopy)
- History of sexually transmitted infections (STIs)
- Multiple sexual partners
- Immunocompromised status
- Poor genital hygiene
Therapeutic Management of Peptostreptococcus Tubo-Ovarian Abscess
Effective treatment of TOA requires prompt antibiotic therapy targeting anaerobic flora and, in many cases, surgical or radiologic intervention.
Empiric Antimicrobial Therapy
Initial management should not wait for culture confirmation. Antibiotics should be active against anaerobes and facultative gram-negative rods.
Preferred Regimens:
- IV Cefoxitin + Doxycycline + Metronidazole
- IV Clindamycin + Gentamicin
- Ampicillin-Sulbactam + Doxycycline
- Carbapenems (e.g., Ertapenem, Meropenem) for resistant or severe cases
Therapy is typically continued for minimum 14 days, transitioning from IV to oral based on clinical response.
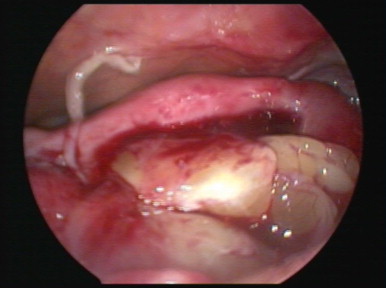
Interventional Drainage or Surgery
Indications for procedural intervention include:
- Abscess >9 cm or not responding to antibiotics within 72 hours
- Evidence of rupture or generalized peritonitis
- Recurrence or chronic TOA
- Suspected malignancy
Drainage Approaches:
- Transvaginal ultrasound-guided aspiration
- CT-guided percutaneous drainage
- Laparoscopic drainage or salpingo-oophorectomy in select cases
Complications Arising from Inadequately Treated TOA
Delayed or ineffective treatment of Peptostreptococcus tubo-ovarian abscess can lead to life-threatening complications and long-term sequelae.
Major Complications
- Rupture of abscess leading to peritonitis or sepsis
- Infertility due to tubal scarring and obstruction
- Chronic pelvic pain
- Adhesion formation causing bowel obstruction
- Pelvic thrombophlebitis
- Tubo-ovarian complex becoming nonresponsive to antibiotics, necessitating surgery
- Ectopic pregnancy in future due to tubal damage
Prevention Strategies and Public Health Considerations
Preventing tubo-ovarian abscesses, especially those involving anaerobes like Peptostreptococcus, requires a combination of education, early intervention, and sexual health practices.
Preventive Measures
- Timely treatment of lower genital tract infections
- Routine STI screening in sexually active individuals
- Proper insertion technique and monitoring for IUDs
- Comprehensive PID management protocols
- Post-procedural care after gynecologic interventions
- Public awareness on symptoms prompting early gynecologic consultation
Peptostreptococcus tubo-ovarian abscess represents a complex, often polymicrobial pelvic infection requiring decisive clinical management. The anaerobic nature of Peptostreptococcus spp. contributes to abscess formation and persistence, necessitating both targeted antimicrobial therapy and potential surgical intervention. Early diagnosis, multidisciplinary care, and strategic prevention are essential to reduce morbidity, preserve fertility, and avoid systemic complications. Heightened awareness of this pathogen’s role in pelvic abscesses ensures better outcomes in reproductive health.