Bacteroides osteomyelitis is a rare but significant type of bone infection caused by Bacteroides species, particularly Bacteroides fragilis. These anaerobic, gram-negative bacteria are commonly found in the human gastrointestinal tract and can become pathogenic under certain conditions. The condition often results from the hematogenous spread of bacteria or direct inoculation during trauma or surgery, leading to severe complications if left untreated.
Pathophysiology of Bacteroides Osteomyelitis
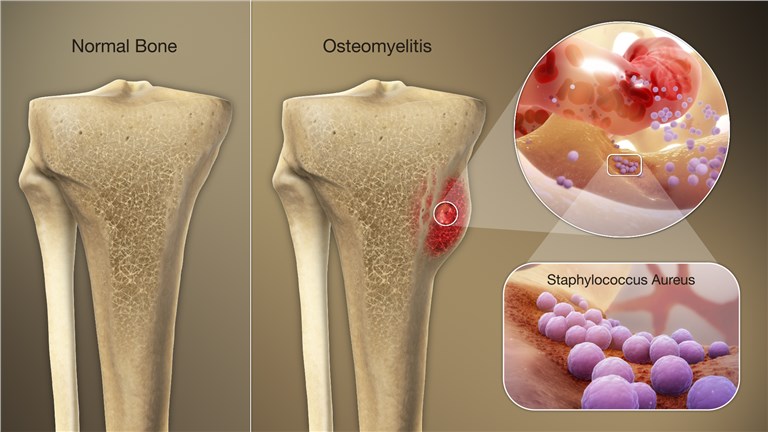
The Bacteroides genus includes opportunistic pathogens that thrive in oxygen-deprived environments. Once these bacteria gain access to bone tissue, they trigger an inflammatory response that compromises bone integrity. The presence of necrotic tissue and abscess formation further facilitates bacterial proliferation and resistance to immune responses.
Key factors include:
Risk Factors for Bacteroides Osteomyelitis
Certain conditions predispose individuals to developing Bacteroides osteomyelitis:
- Surgical Procedures: Orthopedic surgeries with inadequate sterilization.
- Trauma: Open fractures or penetrating injuries.
- Underlying Health Conditions: Diabetes mellitus, peripheral vascular disease, or immunosuppression.
- Contiguous Infection: Spread from nearby infections such as abscesses or ulcers.
Clinical Presentation
The symptoms of Bacteroides osteomyelitis can vary based on the infection site and severity. Common presentations include:
- Localized bone pain and tenderness
- Swelling and erythema over the affected area
- Fever and systemic signs of infection
- Reduced range of motion in adjacent joints
- Formation of draining sinus tracts in chronic cases
Diagnostic Approach
Accurate and timely diagnosis is critical for effective management. The diagnostic process typically involves:
1. Imaging Studies
- X-rays: Identify bone destruction and periosteal reactions.
- MRI: Offers detailed visualization of bone and soft tissue involvement.
- CT Scans: Useful for detecting abscesses or sequestra.
2. Microbiological Testing
- Blood Cultures: May identify bacteremia associated with Bacteroides species.
- Bone Biopsy: Direct sampling of infected bone provides definitive diagnosis and susceptibility testing.
3. Laboratory Tests
- Elevated inflammatory markers such as ESR and CRP
- Leukocytosis in complete blood count (CBC)
Treatment Strategies
Managing Bacteroides osteomyelitis requires a combination of medical and surgical interventions.
1. Antibiotic Therapy
The cornerstone of treatment is prolonged antibiotic therapy tailored to susceptibility profiles:
- First-line Agents: Metronidazole, carbapenems, or beta-lactam/beta-lactamase inhibitor combinations.
- Duration: Typically 6-8 weeks, with intravenous administration followed by oral therapy.
2. Surgical Intervention
In cases of extensive infection, surgical management may be necessary:
- Debridement: Removal of necrotic bone and infected tissues.
- Drainage: Management of abscesses to reduce bacterial load.
- Reconstruction: Bone grafting or other reconstructive procedures to restore structural integrity.
3. Supportive Care
- Adequate pain management
- Nutritional support to enhance healing
- Monitoring for complications, including sepsis or chronic osteomyelitis
Prognosis and Complications
The prognosis of Bacteroides osteomyelitis depends on early diagnosis and treatment. Delayed intervention can lead to:
- Chronic osteomyelitis with persistent infection
- Pathological fractures
- Systemic complications such as septicemia
Prevention
Preventative strategies focus on minimizing risk factors:
- Adhering to sterile techniques during surgeries
- Prompt treatment of wounds and infections
- Regular monitoring for high-risk patients