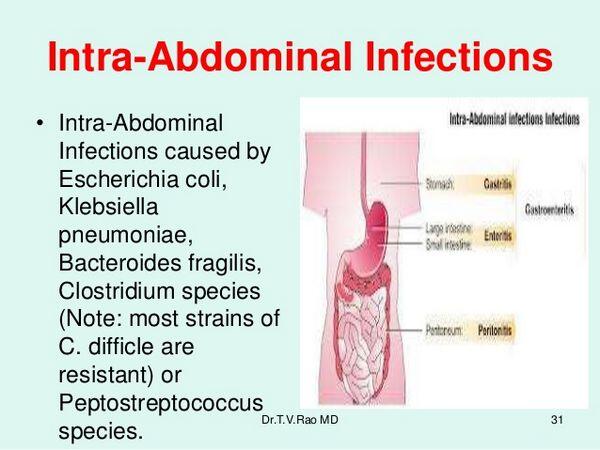
Peptostreptococcus species are gram-positive, anaerobic cocci commonly residing as part of the normal flora in the gastrointestinal tract. Under certain pathological conditions, they transition into opportunistic pathogens, particularly within anaerobic environments such as the peritoneal cavity during episodes of peritonitis. Peptostreptococcus peritonitis represents a significant clinical concern due to its insidious progression, polymicrobial associations, and potential to result in life-threatening intra-abdominal sepsis if not managed promptly.
Pathophysiology of Anaerobic Peritonitis Involving Peptostreptococcus
Peptostreptococcal involvement in peritonitis typically follows gastrointestinal perforation, intra-abdominal surgical contamination, or translocation through inflamed mucosa. The peritoneal cavity, once sterile, becomes a medium for bacterial proliferation, particularly under anaerobic conditions created by necrosis or abscess formation.
Etiology and Risk Factors
Peptostreptococcus contributes significantly to secondary peritonitis, where infection results from intra-abdominal events. It rarely causes primary peritonitis on its own but may be involved in immunocompromised states or patients undergoing peritoneal dialysis.
Common Predisposing Factors
- Gastrointestinal tract perforation (e.g., from ulcers, diverticulitis, appendicitis)
- Postoperative abdominal infection
- Peritoneal dialysis catheter contamination
- Pelvic inflammatory disease
- Pancreatic necrosis or pseudocyst infection
- Inflammatory bowel disease flares
- Immunosuppression (HIV, malignancy, diabetes)
Clinical Manifestations of Peptostreptococcus Peritonitis
The clinical picture is often indistinct from other forms of peritonitis but may evolve more slowly due to the anaerobic nature of the pathogen. Hallmark features include:
- Severe abdominal pain and tenderness
- Abdominal rigidity and rebound tenderness
- Fever, chills, and systemic signs of sepsis
- Nausea, vomiting, and ileus
- Hypotension in advanced infection
- Cloudy peritoneal dialysate (in dialysis-associated peritonitis)
Diagnostic Workup
Accurate identification of Peptostreptococcus peritonitis is crucial due to the need for anaerobic-specific antimicrobial therapy and possible surgical intervention.
Laboratory Investigations
- CBC: Leukocytosis with left shift
- CRP/ESR: Elevated inflammatory markers
- Blood cultures: May be positive in septic cases
- Peritoneal fluid analysis: High WBC count, low glucose, elevated protein
- Anaerobic cultures: Essential for isolating Peptostreptococcus spp.
- Gram stain: May show gram-positive cocci in chains
Imaging Modalities
- Abdominal X-ray: May reveal free air if perforation present
- Ultrasound: Useful for identifying fluid collections and abscesses
- CT Scan (Abdomen and Pelvis): Gold standard for detecting intra-abdominal abscesses, organ perforation, or fluid tracking
Microbiology: Peptostreptococcus in Polymicrobial Infections
Peptostreptococcus rarely acts in isolation. It is typically part of a polymicrobial infection involving both aerobic and anaerobic bacteria.
Frequently Associated Pathogens
- Bacteroides fragilis
- Fusobacterium spp.
- Clostridium spp.
- Escherichia coli
- Enterococcus faecalis
- Klebsiella pneumoniae
Such microbial synergy leads to tissue necrosis, gas formation, and worsening inflammation, increasing the risk of abscess development and septic shock.
Management Strategies for Peptostreptococcus Peritonitis
Timely antimicrobial therapy, source control, and supportive care form the triad of effective peritonitis management.
Empiric Antimicrobial Therapy
Initial broad-spectrum coverage is essential before culture results are available. Effective regimens include:
- Piperacillin-Tazobactam
- Carbapenems (e.g., Meropenem, Imipenem)
- Metronidazole (IV or oral) for specific anaerobic coverage
- Clindamycin (less favored due to increasing resistance)
- Combination of Ceftriaxone + Metronidazole for moderate cases
Once Peptostreptococcus is confirmed, antibiotic therapy should continue for 10–14 days, adjusted based on clinical response and susceptibility.
Surgical Intervention
In many cases, antimicrobial therapy alone is insufficient. Surgical management may include:
- Laparotomy or laparoscopy for source control
- Abscess drainage (percutaneous or open)
- Repair of gastrointestinal perforations
- Catheter removal/replacement in dialysis-related infections
Prognosis and Complications
Prompt diagnosis and aggressive management generally yield good outcomes. However, complications may arise due to the virulence of anaerobic bacteria and delay in initiating appropriate therapy.
Potential Complications
- Septic shock
- Multiorgan dysfunction syndrome (MODS)
- Abdominal compartment syndrome
- Recurrent intra-abdominal abscesses
- Adhesions and bowel obstruction
- Peritoneal fibrosis in chronic or dialysis-associated cases
Preventive Measures and Risk Reduction
Efforts to prevent Peptostreptococcus-related peritonitis are especially important in surgical and dialysis patients.
- Strict aseptic technique during abdominal and peritoneal procedures
- Timely management of GI perforations or inflammatory conditions
- Antibiotic prophylaxis in high-risk surgeries
- Patient education on proper peritoneal dialysis hygiene
- Routine surveillance and catheter care protocols
Peptostreptococcus peritonitis is a serious intra-abdominal infection that requires a high index of suspicion, particularly in polymicrobial or anaerobic infections. As part of the gut flora, Peptostreptococcus spp. can lead to life-threatening peritoneal inflammation when translocated into the peritoneal cavity. Accurate diagnosis, aggressive antimicrobial therapy, and prompt surgical management are key to preventing severe complications and ensuring favorable outcomes.