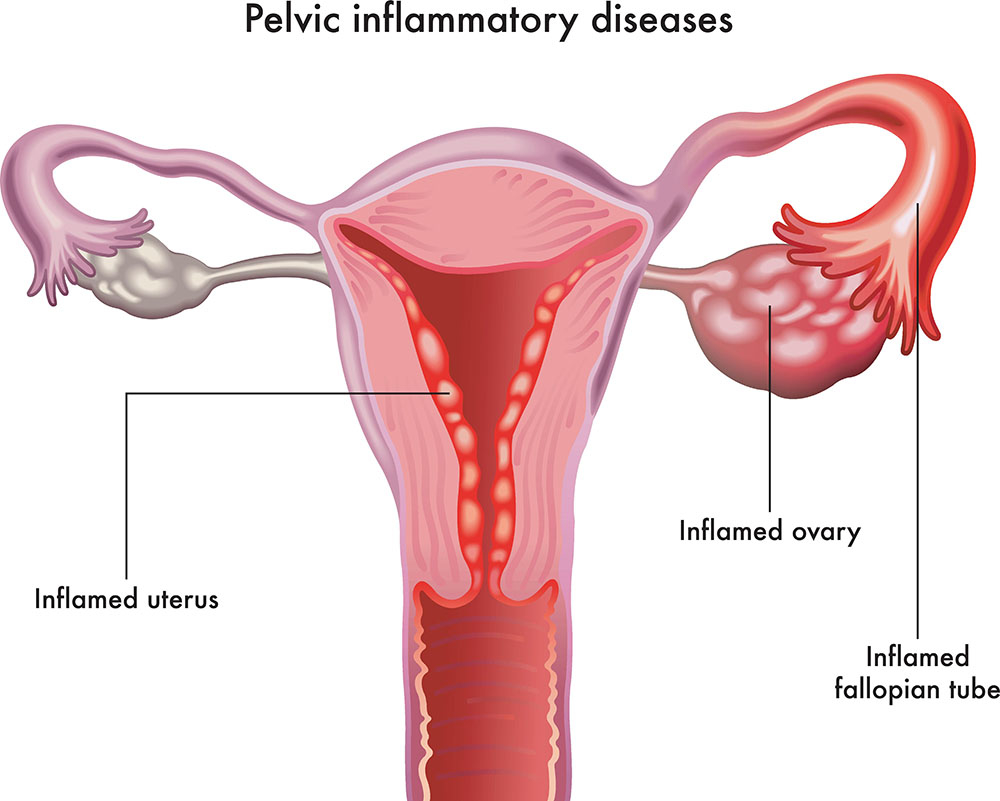
Peptococcus pelvic inflammatory disease (PID) is a complex gynecological condition caused by the invasion of anaerobic gram-positive cocci from the genus Peptococcus into the female reproductive tract. These bacteria, normally part of the vaginal and gastrointestinal flora, become pathogenic under favorable conditions such as mucosal trauma, altered microbiota, or compromised immunity. This anaerobic form of PID often leads to severe pelvic complications, including tubo-ovarian abscesses, infertility, and chronic pelvic pain.
Etiology: How Peptococcus Causes Pelvic Inflammation
Peptococcus-induced PID is primarily endogenous, meaning it originates from the patient’s own flora. It is frequently associated with polymicrobial infections, commonly coexisting with Bacteroides, Prevotella, or facultative anaerobes such as E. coli. Invasive procedures or infections that alter the vaginal pH and oxygen tension facilitate Peptococcus growth and ascent into the upper genital tract.
Predisposing Factors and Risk Profile
Understanding the risk factors is critical in identifying patients vulnerable to anaerobic PID.
Primary Risk Factors:
- Intrauterine device (IUD) insertion without prophylaxis
- Recent childbirth or miscarriage
- Unsafe abortion practices
- Unprotected intercourse with multiple partners
- History of bacterial vaginosis
- Douching and alteration of normal vaginal flora
- Pelvic surgery or gynecologic instrumentation
- Immunocompromised state
Clinical Presentation of Peptococcus-Related PID
Patients with Peptococcus PID typically present with subacute to acute pelvic symptoms, often mimicking other gynecologic disorders.
Common Signs and Symptoms:
- Bilateral lower abdominal or pelvic pain
- Abnormal vaginal discharge with foul odor
- Irregular menstruation or post-coital bleeding
- Fever (>38.3°C) and systemic malaise
- Dyspareunia (pain during intercourse)
- Cervical motion and adnexal tenderness
- Nausea and vomiting (in severe cases)
- Elevated inflammatory markers
Due to the anaerobic nature of Peptococcus, the infection tends to progress insidiously and may form localized abscesses if not promptly treated.
Diagnostic Approach to Anaerobic PID
A comprehensive diagnostic workup is vital for confirming Peptococcus as a causative organism and ruling out other potential sources of pelvic inflammation.
Clinical Assessment:
- Detailed gynecological and sexual history
- Pelvic examination revealing cervical and adnexal tenderness
- Bimanual examination showing uterine mobility pain
Laboratory Investigations:
- Complete blood count (CBC): Neutrophilic leukocytosis
- CRP and ESR: Elevated in active inflammation
- Endocervical swabs and culture: Anaerobic transport medium required
- Gram stain: Shows gram-positive cocci in clusters
- NAATs: To exclude co-infections like Chlamydia and Neisseria
Imaging Studies:
- Pelvic ultrasound: First line to detect tubo-ovarian abscess
- CT or MRI of the pelvis: Useful for evaluating deep tissue involvement, especially when the clinical exam is inconclusive
Microbiological Features of Peptococcus
Peptococcus is a genus of gram-positive, non-spore-forming, anaerobic cocci. It is distinguished from Peptostreptococcus by its slightly more pathogenic profile and resistance to several beta-lactam antibiotics.
Important Characteristics:
- Anaerobic growth requirement
- Commonly isolated with mixed flora
- Often found in abscesses and necrotic tissue
- Exhibits resistance to macrolides and variable susceptibility to penicillins
Management of Peptococcus-Induced PID
Timely and comprehensive management is essential to prevent irreversible pelvic damage and systemic complications.
Empiric Antibiotic Regimen:
Since anaerobes are rarely isolated early, empiric treatment should cover both aerobic and anaerobic bacteria. Once Peptococcus is identified, the regimen may be refined accordingly.
Recommended Antibiotics:
- Clindamycin + Gentamicin: IV combination targeting anaerobes
- Metronidazole + Ceftriaxone + Doxycycline: Standard PID triple therapy
- Ampicillin-Sulbactam or Piperacillin-Tazobactam: In severe polymicrobial infections
Oral Step-Down Therapy (after 48–72 hours of improvement):
- Metronidazole 500 mg PO BID + Doxycycline 100 mg PO BID for 14 days
Surgical Interventions:
- Drainage of pelvic abscess (percutaneous or laparoscopic)
- Hysterectomy or salpingectomy in refractory or necrotizing infections
- Laparoscopy to lyse adhesions and prevent chronic pain syndromes
Potential Complications of Untreated Anaerobic PID
Peptococcus pelvic infections, when neglected, can progress to life-altering sequelae.
Major Complications:
- Tubo-ovarian abscess rupture
- Chronic pelvic pain
- Infertility due to tubal scarring
- Fitz-Hugh–Curtis syndrome (perihepatitis)
- Ectopic pregnancy
- Pelvic peritonitis and septic shock
Prompt therapy significantly reduces the risk of these adverse outcomes.
Prevention of Peptococcus-Associated PID
Preventive strategies target modifying risk behavior, ensuring procedural asepsis, and promptly treating lower genital infections.
Preventive Measures:
- Barrier contraception and limiting sexual partners
- Routine STI screening and treatment
- Avoidance of unnecessary IUD insertion during active infection
- Prophylactic antibiotics for gynecologic surgeries
- Education on reproductive tract hygiene
Peptococcus pelvic inflammatory disease is a serious anaerobic infection requiring vigilant diagnosis and multidisciplinary management. Although underdiagnosed due to culturing difficulties, it remains a clinically significant pathogen in pelvic infections. With increasing antibiotic resistance and complexity of pelvic microbiota, clinicians must maintain a high index of suspicion when evaluating PID cases unresponsive to standard therapy. Through early detection, appropriate anaerobic coverage, and aggressive complication management, we can reduce morbidity and preserve reproductive health in affected individuals.