Peptococcus joint infection refers to a rare but serious form of septic arthritis caused by Peptococcus species, obligate anaerobic gram-positive cocci. These pathogens, particularly Peptococcus niger, are part of the normal mucocutaneous flora but can cause severe infections when they enter sterile sites such as the synovial joint space. Unlike aerobic bacteria, their anaerobic nature demands specialized culture techniques and targeted antibiotic therapy for effective eradication.
Etiology and Risk Factors: How Peptococcus Invades the Joint Space
Peptococcus species typically gain access to the joint via hematogenous spread, direct inoculation, or contiguous extension from nearby infections. Their growth is favored in low-oxygen environments often found in necrotic or poorly perfused tissues.
Predisposing Risk Factors:
- Prosthetic joint implants
- Open joint trauma or puncture wounds
- Immunosuppression (e.g., HIV, corticosteroids)
- Rheumatoid arthritis or pre-existing joint disease
- Recent joint surgery or aspiration
- Poor dental hygiene (via hematogenous bacteremia)
Pathogenesis: Development of Anaerobic Septic Arthritis by Peptococcus
Peptococcus species initiate infection through colonization of synovial fluid, followed by enzymatic degradation of cartilage, immune cell infiltration, and pus formation. Due to the avascular nature of cartilage, antibiotic penetration is limited, often requiring surgical drainage for definitive management.
Infections progress rapidly and can lead to irreversible joint damage within days if left untreated.
Clinical Manifestations of Peptococcus-Induced Septic Arthritis
Early diagnosis relies on recognizing the characteristic features of anaerobic joint infections. Symptoms are often monoarticular but can involve multiple joints in immunocompromised patients.
Common Symptoms:
- Acute joint pain and swelling
- Warmth and erythema over affected joint
- Restricted range of motion
- Fever and malaise
- Purulent joint effusion
- Pain exacerbated by passive or active movement
The knee is most commonly affected, followed by hip, shoulder, and elbow joints.
Diagnostic Approach: Confirming Peptococcus Joint Infection
Accurate diagnosis requires a combination of clinical, laboratory, and imaging assessments. Given the anaerobic nature of Peptococcus, special handling of specimens is crucial.
Laboratory Investigations:
- Synovial Fluid Analysis
- Appearance: turbid or purulent
- WBC count: >50,000/mm³ with neutrophilic predominance
- Glucose: markedly reduced
- Gram stain: gram-positive cocci in clusters (may be sparse)
- Anaerobic Culture of Synovial Fluid
- Requires collection in anaerobic transport media
- May take 48–72 hours for growth
- Peptococcus is catalase-negative and indole-negative
- Blood Cultures
- Positive in hematogenous spread
- Should include anaerobic bottles
- Inflammatory Markers
- Elevated CRP, ESR, and procalcitonin
Imaging:
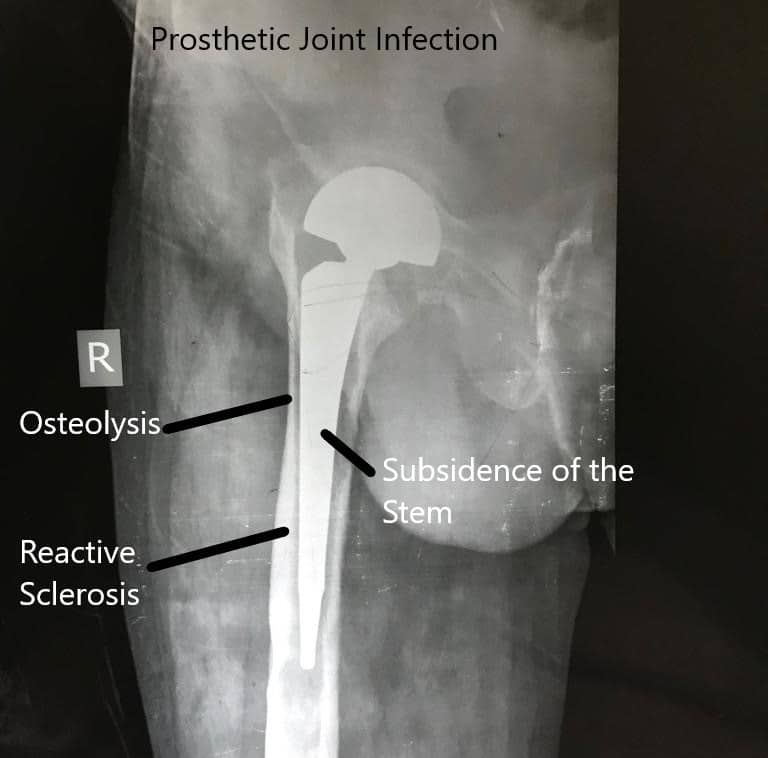
- X-ray: May show joint space narrowing or erosions in advanced stages
- Ultrasound: Detects effusion or synovial thickening
- MRI: Best for early detection of bone involvement or abscesses
Differential Diagnosis: Distinguishing Peptococcus Joint Infection from Other Arthropathies
Due to overlapping symptoms, anaerobic septic arthritis must be differentiated from other joint conditions.
| Condition | Distinguishing Features |
|---|---|
| Gout or Pseudogout | Presence of crystals in synovial fluid |
| Rheumatoid Arthritis | Symmetric joint involvement, chronic symptoms |
| Osteoarthritis | Gradual onset, non-inflammatory effusion |
| Tuberculous Arthritis | Chronic monoarthritis with caseating granulomas |
| Other Septic Arthritis (Staph/Strep) | Rapid culture positivity in aerobic media |
Treatment Protocol: Eradicating Anaerobic Peptococcus from Joints
Successful management hinges on a dual approach—prompt antibiotic therapy and joint drainage.
Empirical Antibiotic Therapy:
- Clindamycin 600–900 mg IV every 8 hours
- Metronidazole 500 mg IV every 8 hours
- Penicillin G 4 million units IV every 4 hours (if sensitive)
- Ampicillin-sulbactam 3 g IV every 6 hours as alternative
Following identification of Peptococcus, therapy is adjusted based on sensitivity.
Duration of Antibiotic Treatment:
- 2 to 4 weeks IV therapy, followed by oral antibiotics if needed
- Total duration: 4 to 6 weeks, depending on clinical response and imaging
Surgical Interventions:
- Arthroscopic lavage or open arthrotomy for joint washout
- Synovectomy in persistent synovitis
- Prosthesis removal in prosthetic joint infections (with reimplantation after eradication)
Prognosis and Long-Term Outcomes
When diagnosed early and treated appropriately, prognosis is favorable. Delayed management may result in:
- Permanent joint dysfunction
- Osteomyelitis
- Septicemia
- Chronic pain and mobility limitations
- Joint ankylosis
Patients with comorbidities such as diabetes or immunosuppression have higher complication risks.
Preventive Measures for Anaerobic Septic Arthritis
Preventing Peptococcus joint infections involves stringent aseptic techniques and early management of risk factors.
Preventive Strategies:
- Strict sterility in joint injections and surgeries
- Dental hygiene to prevent hematogenous seeding
- Prompt treatment of nearby skin or soft tissue infections
- Careful follow-up of prosthetic joints
- Immunization (e.g., pneumococcal vaccine) in high-risk individuals
Peptococcus joint infection, though uncommon, is a critical form of anaerobic septic arthritis requiring urgent attention. Its diagnosis is often delayed due to non-specific symptoms and slow anaerobic culture growth. Clinicians must maintain a high index of suspicion, especially in patients with prosthetic joints or immunosuppression. Early empirical anaerobic coverage, surgical drainage, and targeted therapy are key to preventing irreversible joint destruction and systemic complications.