Peptococcus endometritis is a rare yet clinically significant infection of the endometrial lining caused by anaerobic gram-positive cocci, primarily of the genus Peptococcus. These anaerobic bacteria are part of the normal flora of mucosal surfaces but can become pathogenic in conditions that disrupt the microbial balance of the female reproductive tract. The condition often presents as part of polymicrobial endometritis or pelvic inflammatory disease (PID), posing diagnostic and therapeutic challenges due to its insidious progression and anaerobic nature.
Etiology: Anaerobic Pathogens and Their Role in Endometrial Infection
The Peptococcus species, especially Peptococcus niger, thrive in anaerobic environments such as necrotic or poorly perfused uterine tissue. Infection typically arises following:
- Postpartum or post-abortion procedures
- Intrauterine device (IUD) insertion
- Unsterile gynecological interventions
- Secondary infections following Cesarean delivery
The pathogens gain access through ascending routes, colonize the endometrium, and proliferate in the anaerobic environment created by retained placental fragments or necrotic debris.
Pathogenesis: Progression of Peptococcus-Related Endometrial Inflammation
The pathophysiology of Peptococcus endometritis involves several key steps:
Due to the anaerobic growth requirements, Peptococcus infections are often missed by conventional aerobic cultures, delaying diagnosis and treatment.
Clinical Presentation: Signs and Symptoms of Peptococcus Endometritis
Peptococcus endometritis typically manifests with signs consistent with acute or chronic uterine infection. Recognizing early indicators is critical for timely intervention.
Common Symptoms:
- Pelvic pain or lower abdominal tenderness
- Abnormal uterine bleeding (intermenstrual or postcoital)
- Purulent or foul-smelling vaginal discharge
- Fever and systemic signs of infection
- Dyspareunia (pain during intercourse)
- Uterine tenderness on bimanual examination
In advanced cases, patients may develop peritonitis, tubo-ovarian abscess, or bacteremia, particularly if the infection remains untreated.
Diagnostic Evaluation of Anaerobic Endometritis
Diagnosis relies on a combination of clinical findings, laboratory tests, and imaging modalities. Due to the anaerobic nature of Peptococcus, specialized microbiological techniques are essential.
Key Diagnostic Steps:
- Endometrial Biopsy and Culture
Samples must be cultured under anaerobic conditions to detect Peptococcus niger or related species. - Transvaginal Ultrasound
Identifies endometrial thickening, retained products of conception, or intrauterine abscesses. - Complete Blood Count (CBC)
Elevated white blood cell count with neutrophilia may indicate systemic infection. - C-reactive Protein (CRP) and ESR
Serve as inflammatory markers in subacute or chronic cases. - Pelvic MRI (in complex or recurrent cases)
Offers superior soft tissue resolution for detecting complications like abscesses or deep pelvic spread.
Treatment Protocols for Peptococcus Endometritis
Early empirical treatment followed by tailored antibiotic therapy is essential to eradicate infection and prevent complications.
Empirical Antibiotic Therapy
- First-line Regimen:
- Clindamycin + Gentamicin (covers anaerobes and gram-negative aerobes)
- Alternative Regimens:
- Metronidazole combined with Ampicillin-sulbactam
- Cefoxitin plus Doxycycline
Targeted Therapy
Once Peptococcus is identified:
- Switch to high-dose Metronidazole (500 mg IV/oral every 8 hours) for 10–14 days
- Monitor clinical improvement; extend duration for complicated infections
Surgical Management
- Uterine evacuation may be required if retained products of conception are present
- Laparoscopic drainage for tubo-ovarian abscesses
- Hysterectomy considered only in refractory or recurrent severe infections in non-fertile patients
Prognosis and Outcomes
With prompt diagnosis and appropriate antimicrobial therapy, most patients recover fully without long-term sequelae. However, delayed treatment increases the risk of:
- Chronic pelvic pain
- Infertility due to tubal scarring
- Sepsis and multi-organ dysfunction
Preventive Measures and Risk Reduction
Preventive strategies focus on reducing exposure to anaerobic pathogens and ensuring sterile procedural environments.
Key Preventive Actions:
- Adherence to sterile techniques during gynecologic interventions
- Judicious use and proper monitoring of IUDs
- Prompt postpartum care to ensure complete expulsion of placental tissue
- Prophylactic antibiotics during abortion procedures or Cesarean delivery
- Early treatment of bacterial vaginosis, which may harbor anaerobic pathogens including Peptococcus
Differential Diagnosis
Given the non-specific presentation, Peptococcus endometritis must be distinguished from other gynecological conditions:
| Condition | Differentiating Features |
|---|---|
| Pelvic Inflammatory Disease | Often polymicrobial; may include aerobic bacteria |
| Endometrial Carcinoma | Postmenopausal bleeding, abnormal Pap smear |
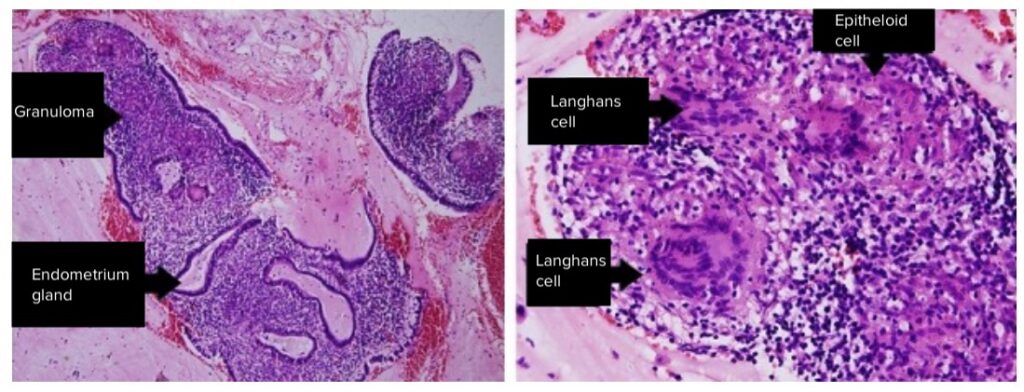
| Tuberculosis Endometritis | Granulomatous histology, history of TB exposure |
| Actinomyces Infection | Often linked with IUD use; sulfur granules present |
Peptococcus endometritis represents a rare but significant anaerobic infection of the endometrium, frequently overlooked due to its diagnostic complexity. A multidisciplinary approach—combining clinical suspicion, anaerobic culture techniques, imaging, and effective antibiotic regimens—ensures successful management. Preventive strategies and awareness of post-interventional risks are key to minimizing occurrence and ensuring long-term reproductive health.