Bacteroides liver abscess is a serious medical condition caused primarily by anaerobic bacteria, such as Bacteroides fragilis. These bacteria are part of the normal flora in the gastrointestinal tract but can cause significant infections when translocated to the liver. Understanding the pathophysiology, risk factors, clinical presentation, and management of this condition is essential for effective treatment.
Pathophysiology of Bacteroides Liver Abscess
A liver abscess occurs when pathogens invade liver tissue, leading to localized inflammation and pus formation. Bacteroides species, particularly Bacteroides fragilis, play a prominent role due to their ability to:
- Resist phagocytosis through capsular polysaccharides.
- Produce enzymes such as proteases that degrade host tissue.
- Develop biofilms, which contribute to antimicrobial resistance.
Abscess formation typically results from the hematogenous spread of bacteria or direct extension from nearby infections.
Causes and Risk Factors
The development of Bacteroides liver abscess is multifactorial, involving:
Common Causes
- Hematogenous Spread: Through the portal vein from gastrointestinal infections, particularly diverticulitis, appendicitis, or perforated bowel.
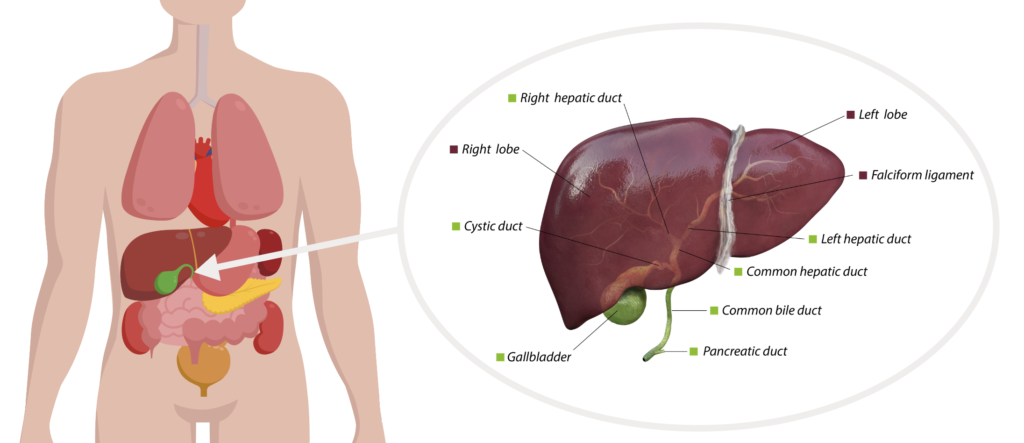
- Direct Extension: From adjacent structures such as the biliary tree in cases of cholangitis.
- Trauma or Surgery: Liver trauma or surgical procedures can introduce anaerobic bacteria.
Risk Factors
- Immunosuppression (e.g., HIV, chemotherapy, corticosteroids)
- Diabetes mellitus
- Malignancies of the gastrointestinal tract
- Chronic liver diseases, including cirrhosis
Clinical Presentation
Patients with a Bacteroides liver abscess often present with nonspecific symptoms, including:
- Fever and chills (present in over 90% of cases)
- Right upper quadrant abdominal pain
- Jaundice (in severe or biliary-associated cases)
- Anorexia and unintentional weight loss
- Fatigue and malaise
Complications may include sepsis, rupture of the abscess into the peritoneal cavity, and metastatic infections.
Diagnosis
Accurate diagnosis requires a combination of clinical evaluation, laboratory testing, and imaging studies.
Laboratory Findings
- Elevated white blood cell count with neutrophilia
- Elevated liver enzymes (ALT, AST, ALP, and bilirubin)
- Positive blood cultures for anaerobic bacteria
Imaging Studies
- Ultrasound: Initial imaging modality to detect hypoechoic lesions.
- CT Scan: More sensitive in identifying abscess size, location, and number.
- MRI: Occasionally used for detailed liver imaging.
Microbiological Analysis
Aspiration of abscess fluid under ultrasound or CT guidance is crucial for identifying causative organisms and determining antibiotic susceptibility.
Treatment Strategies
Antibiotic Therapy
Empiric antibiotic treatment should target anaerobic organisms and gram-negative facultative bacteria. Common regimens include:
- Metronidazole combined with ceftriaxone or piperacillin-tazobactam.
- Monotherapy with carbapenems (e.g., meropenem).
Duration: Typically 4-6 weeks, with adjustments based on clinical response and imaging follow-up.
Percutaneous Drainage
Ultrasound- or CT-guided percutaneous drainage is often the first-line intervention for abscesses larger than 3 cm. This minimally invasive procedure significantly improves patient outcomes when combined with antibiotic therapy.
Surgical Intervention
Indicated in cases where percutaneous drainage is not feasible or complications such as rupture into the peritoneal cavity occur.
Prevention and Prognosis
Prevention
- Early treatment of underlying gastrointestinal or biliary infections
- Adequate surgical asepsis
- Timely management of chronic diseases like diabetes
Prognosis
With prompt diagnosis and treatment, the prognosis is favorable. Delayed intervention can result in higher morbidity and mortality due to complications such as sepsis or abscess rupture.