Penile carcinoma is a rare but aggressive malignancy primarily affecting the skin and mucosa of the penis. The vast majority of cases are squamous cell carcinoma (SCC), accounting for over 95% of diagnoses. This condition poses significant clinical, psychological, and social challenges due to its location and potential mutilating treatment. Early diagnosis and a multidisciplinary treatment approach are critical for improved survival and quality of life.
Epidemiology and Risk Factors of Penile Cancer
Penile carcinoma is uncommon in developed nations, with an incidence of less than 1 per 100,000 men annually. However, its prevalence is markedly higher in parts of Africa, Asia, and South America due to differing hygiene practices, socioeconomic factors, and access to healthcare.
Key Risk Factors:
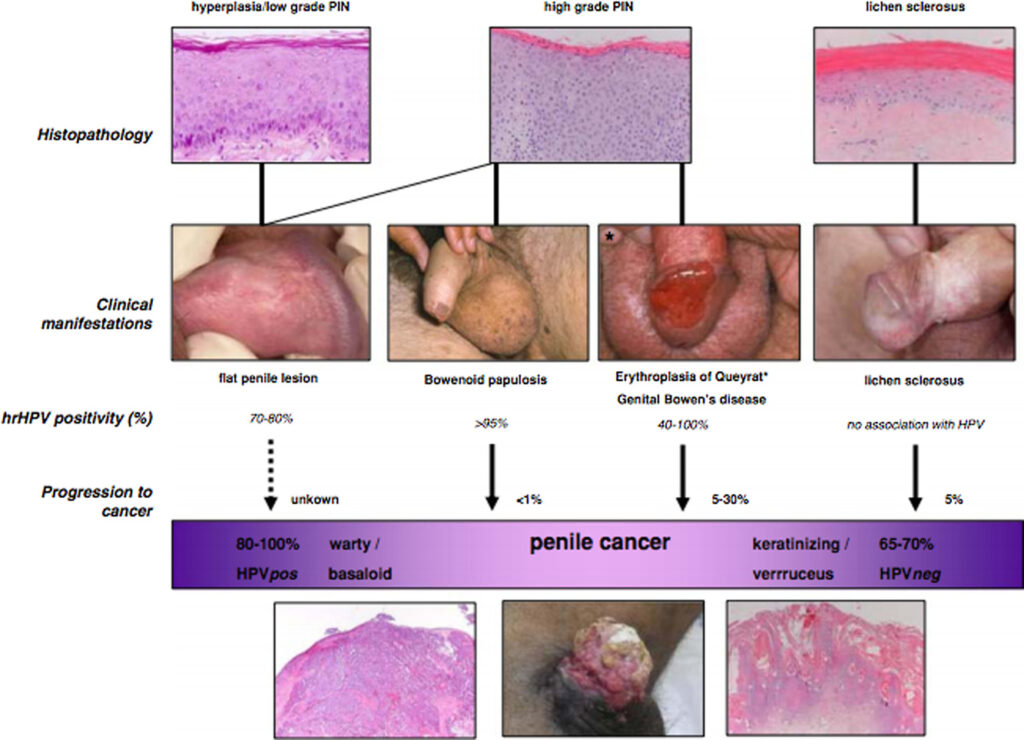
- Human Papillomavirus (HPV) Infection: Especially HPV types 16 and 18
- Phimosis: Chronic inability to retract the foreskin
- Poor Genital Hygiene: Leads to smegma accumulation and chronic inflammation
- Tobacco Use: Strongly associated with carcinogenesis
- Multiple Sexual Partners and early age at first intercourse
- Lichen Sclerosus and other chronic inflammatory penile conditions
- Lack of Circumcision: Associated with higher incidence due to poor hygiene
Pathophysiology and Histological Types
Penile carcinoma typically originates from the epithelial layer of the glans, foreskin, or shaft. Chronic irritation and infection, particularly with oncogenic HPV, result in epithelial dysplasia and eventual malignant transformation.
Histological Subtypes of Penile Squamous Cell Carcinoma:
| Type | Characteristics |
|---|---|
| Usual SCC | Most common; moderate to poorly differentiated |
| Verrucous carcinoma | Exophytic, slow-growing, low metastatic risk |
| Basaloid carcinoma | High-grade, often HPV-associated, aggressive |
| Warty carcinoma | Papillomatous, associated with HPV |
| Papillary carcinoma | Frond-like projections, less aggressive |
| Sarcomatoid carcinoma | Poor prognosis, rare |
Clinical Presentation and Symptoms
Patients typically present with visible or palpable penile lesions. Delay in diagnosis is common due to social stigma or misinterpretation of symptoms.
Common Signs and Symptoms:
- Painless ulcer or growth on the glans, foreskin, or shaft
- Bleeding, discharge, or foul odor
- Pain or swelling in advanced cases
- Inguinal lymphadenopathy (suggesting metastasis)
- Dysuria or obstructive urinary symptoms in late stages
Staging of Penile Carcinoma
Staging follows the TNM classification system (Tumor, Node, Metastasis), which guides treatment planning and prognosis assessment.
Diagnostic Evaluation
Diagnosis of penile carcinoma requires a combination of clinical examination, histopathology, and imaging.
Diagnostic Steps:
- Physical Examination: Inspection and palpation of penile lesion and inguinal lymph nodes.
- Biopsy: Incisional or excisional, mandatory for definitive diagnosis.
- Imaging Studies:
- Ultrasound or MRI for local invasion
- CT scan or PET scan for lymph node and distant metastasis
- HPV Testing: May guide prognosis and future vaccination strategies
Treatment Modalities for Penile Cancer
The therapeutic approach depends on tumor stage, grade, location, and patient preference. A balance between oncologic control and organ preservation is essential.
1. Surgical Management
- Circumcision: For carcinoma in situ or pre-malignant lesions
- Wide Local Excision (WLE): For low-stage tumors, preserving penile function
- Partial Penectomy: For invasive cancers with adequate margin
- Total Penectomy: Reserved for extensive tumors
- Reconstructive Surgery: Using flap or graft techniques to restore form and function
- Inguinal Lymphadenectomy: Based on nodal staging, therapeutic and prognostic
2. Radiotherapy
- External Beam Radiotherapy (EBRT) or Brachytherapy
- Organ-preserving in early stages or palliative in advanced disease
- Associated with complications like urethral stenosis, fibrosis
3. Chemotherapy
- Neoadjuvant chemotherapy: Cisplatin-based regimens for bulky nodal disease
- Adjuvant chemotherapy: Post-surgical in high-risk cases
- Palliative chemotherapy: In metastatic disease
4. Topical and Targeted Therapy
- Topical 5-FU or Imiquimod: For carcinoma in situ
- EGFR inhibitors and immunotherapy: Under investigation for advanced/recurrent disease
Prognosis and Survival Rates
Prognosis is highly dependent on tumor stage and lymph node involvement:
- Localized Disease: >85% 5-year survival
- Regional Nodal Involvement: 50–70%
- Distant Metastases: <10%
Early diagnosis and prompt treatment are the strongest predictors of long-term survival.
Prevention and Public Health Strategies
1. Circumcision in Infancy
Reduces lifetime risk by lowering chances of phimosis and improving hygiene.
2. HPV Vaccination
- Quadrivalent and 9-valent vaccines target oncogenic HPV types.
- Effective in preventing HPV-associated penile neoplasms.
3. Public Awareness and Screening
- Education on genital hygiene, STI prevention, and early signs of cancer.
- Targeting high-risk populations in endemic regions.
Penile carcinoma, while rare, demands prompt recognition and aggressive yet organ-preserving management. Preventive strategies such as HPV vaccination, circumcision, and education are key to reducing incidence. With advancing surgical and systemic therapies, even advanced-stage cases can now achieve meaningful clinical outcomes. A multidisciplinary, evidence-based approach remains the cornerstone for optimal care of penile cancer patients.