Pemphigoid refers to a group of rare autoimmune blistering skin diseases characterized by subepidermal blister formation. These disorders arise when the immune system produces autoantibodies that mistakenly target the skin’s basement membrane, leading to inflammation and separation of the epidermis from the dermis. The disease predominantly affects older adults and can present with varying severity depending on the type and extent of involvement.
Types of Pemphigoid and Their Clinical Distinctions
Bullous Pemphigoid (BP)
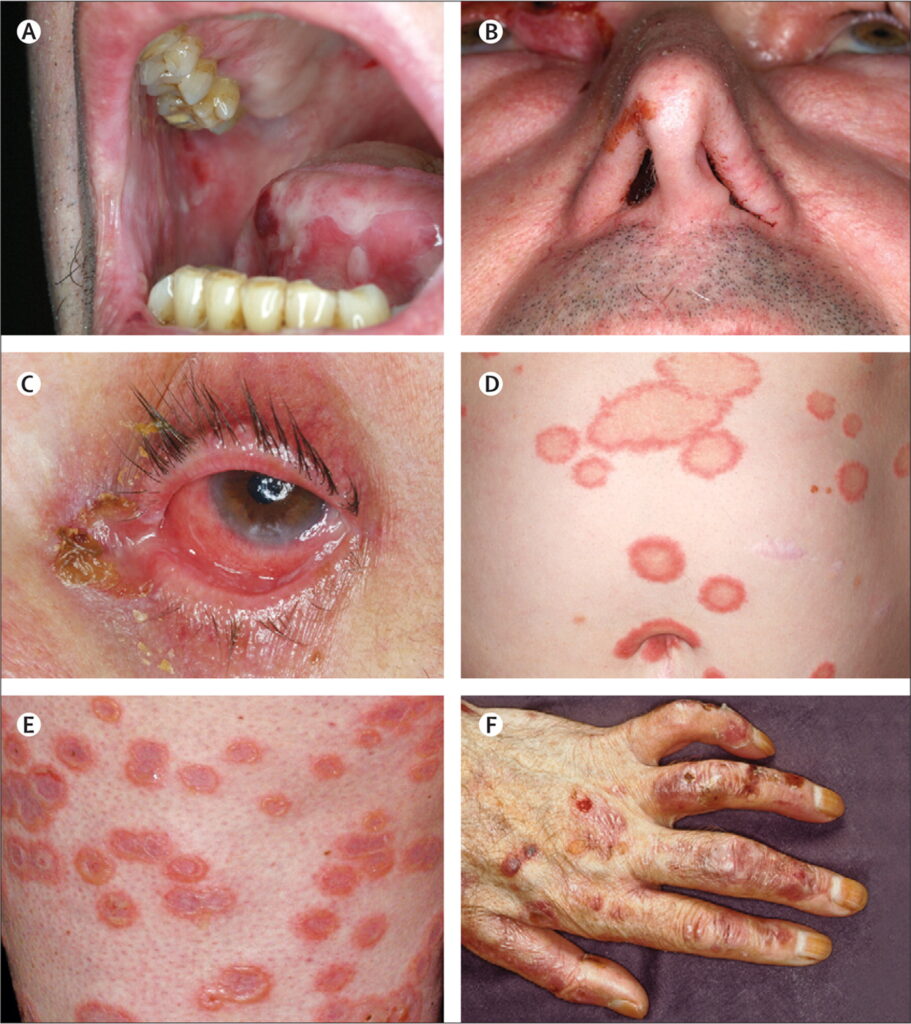
The most common form, bullous pemphigoid, typically affects individuals over 60 and manifests as large, tense blisters on normal or reddened skin, commonly on the trunk, abdomen, and limbs. It is frequently associated with intense pruritus (itchiness) before blistering appears.
Mucous Membrane Pemphigoid (MMP)
MMP, also known as cicatricial pemphigoid, primarily affects mucous membranes such as the oral cavity, eyes, nasopharynx, and genital mucosa. It can lead to scarring and functional impairment, especially in ocular and laryngeal involvement.
Pemphigoid Gestationis
This rare form develops during pregnancy, particularly in the second or third trimester. It resembles bullous pemphigoid in presentation but usually resolves after delivery, although postpartum flares may occur.
Other Variants
- Linear IgA Disease: Characterized by linear IgA deposits at the basement membrane zone.
- Drug-Induced Pemphigoid: Linked to certain medications like loop diuretics and penicillamine.
Pathophysiology: Autoantibody-Mediated Skin Blistering
The pathogenesis involves autoantibodies (primarily IgG) directed against hemidesmosomal proteins such as BP180 (type XVII collagen) and BP230 in the basement membrane zone. These immune complexes trigger complement activation, neutrophil recruitment, and enzymatic degradation of anchoring filaments, resulting in blister formation beneath the epidermis.
Common Signs and Symptoms of Pemphigoid
Cutaneous Manifestations
- Large, tense blisters filled with clear or blood-tinged fluid
- Erythematous or urticarial plaques
- Itching, often intense and persistent
- Erosions or crusting after blisters rupture
Mucosal Involvement
More prominent in mucous membrane pemphigoid:
- Painful oral ulcers
- Conjunctivitis or eye scarring (symblepharon)
- Nasal or genital erosions
- Difficulty swallowing if the esophagus is involved
Diagnostic Approach to Pemphigoid
Clinical Examination
A detailed skin and mucosal exam, along with patient history (age, drug exposure, symptom pattern), forms the diagnostic foundation.
Histopathology
- Skin biopsy from a lesion edge reveals subepidermal blister with eosinophilic infiltration.
Direct Immunofluorescence (DIF)
- A biopsy of perilesional skin shows linear deposition of IgG and/or C3 at the dermoepidermal junction.
Indirect Immunofluorescence (IIF)
- Detects circulating autoantibodies against basement membrane proteins in patient serum.
ELISA Testing
- Identifies and quantifies anti-BP180 and anti-BP230 autoantibodies, supporting diagnosis and monitoring disease activity.
Differential Diagnosis
Pemphigoid must be differentiated from:
- Pemphigus vulgaris (intraepidermal blistering)
- Dermatitis herpetiformis
- Epidermolysis bullosa acquisita
- Linear IgA bullous dermatosis
Correct diagnosis is crucial for appropriate treatment initiation.
Treatment of Pemphigoid: Medical and Supportive Strategies
First-Line Therapy
- Topical corticosteroids for localized/mild disease (e.g., clobetasol)
- Systemic corticosteroids (prednisone) for moderate to severe disease
Immunosuppressive and Immunomodulatory Agents
- Azathioprine
- Mycophenolate mofetil
- Methotrexate
- Dapsone (especially in mucous membrane involvement)
- Tetracyclines with or without nicotinamide in mild disease
Biologic Therapies
For refractory or steroid-dependent cases:
- Rituximab: Anti-CD20 monoclonal antibody
- Omalizumab: Anti-IgE therapy
- IVIG (Intravenous Immunoglobulin): For severe or rapidly progressing disease
Disease Monitoring and Long-Term Management
- Regular follow-up for disease control and medication side effects
- Serologic monitoring of BP180/BP230 antibodies for activity assessment
- Tapering immunosuppressives gradually after remission
- Nutritional and wound care support, especially in elderly patients
- Ophthalmology or ENT referral for mucosal involvement
Prognosis and Potential Complications
- Bullous pemphigoid has a favorable prognosis with treatment but may relapse.
- Mucous membrane pemphigoid can lead to permanent scarring, especially in the eyes and larynx, necessitating early aggressive therapy.
- Secondary skin infections, sepsis, and adverse drug reactions are notable risks in severe or prolonged cases.
Preventive Considerations and Patient Education
- Avoidance of triggering medications
- Early treatment of infections or trauma to the skin
- Patient education on medication adherence
- Monitoring for long-term corticosteroid complications (osteoporosis, hyperglycemia, hypertension)
- Psychosocial support for individuals coping with chronic visible skin conditions
Pemphigoid represents a complex but manageable group of autoimmune blistering disorders, with early diagnosis and individualized treatment being pivotal in reducing morbidity. Multidisciplinary care and long-term monitoring play essential roles in ensuring optimal outcomes for affected individuals. A thorough understanding of the disease mechanisms and clinical presentation is essential for timely intervention and improved patient quality of life.