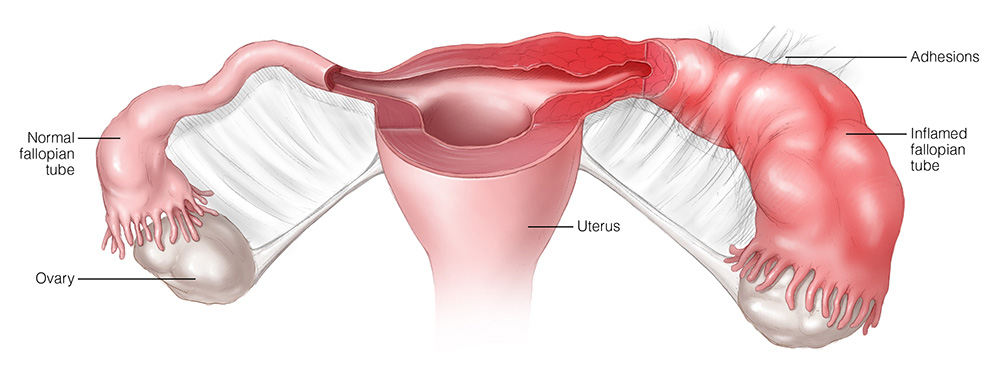
Pelvic Inflammatory Disease (PID) is a severe, ascending infection of the female reproductive tract primarily affecting the uterus, fallopian tubes, and ovaries. Among the pathogens responsible, Neisseria gonorrhoeae remains a leading cause of PID, contributing to considerable reproductive morbidity worldwide. As a sexually transmitted pathogen, N. gonorrhoeae initiates mucosal inflammation that may rapidly progress to involve deeper pelvic structures if left untreated.
Etiology: Role of Neisseria Gonorrhoeae in PID
Neisseria gonorrhoeae is a gram-negative diplococcus with a high affinity for columnar epithelial cells, especially within the endocervix, urethra, and fallopian tubes. Upon infection, it elicits a marked inflammatory response, disrupting epithelial barriers and facilitating polymicrobial superinfection—commonly in conjunction with Chlamydia trachomatis and anaerobic bacteria.
Transmission Pathway
- Unprotected sexual contact with an infected individual
- Ascension of bacteria from cervix to upper genital tract
- Colonization and inflammation of endometrium, salpinges, and ovaries
Risk Factors for PID with Neisseria Gonorrhoeae
- Age under 25 years
- Multiple sexual partners
- Inconsistent condom use
- Previous history of sexually transmitted infections (STIs)
- Recent IUD insertion
- Douching, which alters vaginal flora
Clinical Presentation: Signs and Symptoms
Typical Symptomatology
Patients with PID caused by Neisseria gonorrhoeae often exhibit:
- Lower abdominal and pelvic pain
- Purulent vaginal discharge
- Pain during intercourse (dyspareunia)
- Painful urination (dysuria)
- Fever >38°C
- Irregular menstrual bleeding
- Nausea and vomiting in more severe cases
In some cases, symptoms may be subtle or absent, particularly in early stages, leading to delayed diagnosis and increased risk of complications.
Diagnostic Evaluation of Gonorrhea-Associated PID
Clinical Diagnosis
Diagnosis is primarily clinical, supported by symptom assessment and pelvic examination:
- Cervical motion tenderness
- Adnexal tenderness
- Uterine tenderness
Presence of these three findings warrants empirical treatment.
Laboratory Investigations
- Nucleic Acid Amplification Tests (NAATs) for N. gonorrhoeae and C. trachomatis
- Microscopy: Polymorphonuclear leukocytes in endocervical or urethral discharge
- Culture: For antibiotic sensitivity profiling
- Pregnancy test: To rule out ectopic pregnancy
- CRP and ESR: May be elevated
Imaging Studies
- Transvaginal Ultrasound: To assess tubo-ovarian abscesses or fluid accumulation
- MRI/CT Scan: For complicated or recurrent infections
Standard Treatment Protocols
Empiric Antimicrobial Therapy
Due to the polymicrobial nature of PID, empiric broad-spectrum therapy is recommended. Treatment must cover:
- Neisseria gonorrhoeae
- Chlamydia trachomatis
- Anaerobes and facultative organisms
CDC-Recommended Regimen:
- Ceftriaxone 500 mg IM single dose (or 1g if >150 kg)
- Doxycycline 100 mg orally twice daily for 14 days
- Metronidazole 500 mg orally twice daily for 14 days
Hospitalization Criteria
Inpatient treatment is required if:
- Severe illness or high fever
- Suspected or confirmed tubo-ovarian abscess
- Pregnancy
- Non-response to oral therapy
- Inability to tolerate outpatient medications
Potential Complications of Untreated Gonorrheal PID
- Infertility due to fallopian tube scarring
- Ectopic pregnancy
- Chronic pelvic pain
- Fitz-Hugh–Curtis syndrome (perihepatitis)
- Tubo-ovarian abscess
- Recurrent PID episodes
Prompt diagnosis and full adherence to treatment significantly reduce the risk of permanent damage to reproductive organs.
Prevention Strategies
Primary Prevention
- Consistent condom use
- Regular STI screening, particularly in sexually active women under 25
- Prompt partner notification and treatment
- Limiting number of sexual partners
- Public health education on STI risks
Secondary Prevention
- Early identification of asymptomatic gonorrheal infections
- Post-treatment follow-up to confirm eradication
- Abstinence during treatment to prevent re-infection
- Partner therapy to reduce transmission cycle
Special Considerations in Adolescents and Pregnant Women
Adolescents
Young women are particularly susceptible due to immature cervical epithelium. Emphasis should be placed on comprehensive sex education, early screening, and confidential access to treatment.
Pregnancy
PID during pregnancy is rare but extremely dangerous. Immediate hospitalization and parenteral antibiotics are mandatory due to risks of preterm labor, fetal loss, or maternal sepsis.
Follow-up and Long-Term Management
- Re-evaluate patient within 48–72 hours of initiating therapy
- Test-of-cure is not necessary for gonorrhea unless symptoms persist
- Repeat testing in 3 months post-treatment due to high re-infection rates
- Educate patients on recognizing recurrence or complications
- Discuss fertility planning in those with repeated infections
Pelvic Inflammatory Disease caused by Neisseria gonorrhoeae remains a major public health challenge with lasting consequences if not managed promptly. Clinicians must maintain high suspicion in at-risk individuals and initiate treatment early to prevent complications. Comprehensive care, including partner management and education, is vital to reduce recurrence and protect reproductive health.