Pelvic cellulitis is a serious bacterial infection that affects the soft tissues within the pelvic region. It involves the subcutaneous tissue and dermis, and may extend deeper into surrounding organs or tissues if left untreated. This condition most frequently arises as a complication of gynecological procedures, postpartum infections, or pelvic surgeries. Rapid medical intervention is essential to prevent systemic spread and life-threatening outcomes.
Understanding the Pathophysiology of Pelvic Cellulitis
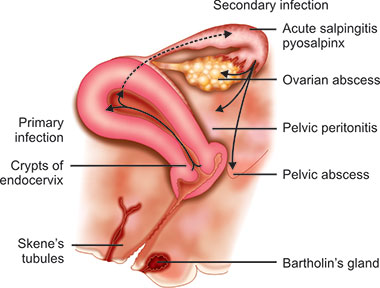
Pelvic cellulitis typically results from the infiltration of pathogenic bacteria—most commonly Streptococcus pyogenes and Staphylococcus aureus—through breaches in the skin or mucosal barriers. Once bacteria penetrate the protective layers, they trigger an acute inflammatory response, causing edema, warmth, erythema, and severe pain in the pelvic region.
Common Routes of Infection
- Post-surgical wounds (e.g., hysterectomy, C-section)
- Vaginal or cervical lacerations
- Pelvic trauma
- Perineal infections
- Extension from urinary tract or rectal infections
High-Risk Factors for Pelvic Cellulitis
Several conditions and procedures predispose individuals to pelvic cellulitis:
- Cesarean section and vaginal delivery
- Pelvic or abdominal surgeries
- Diabetes mellitus
- Obesity
- Immunosuppression
- Poor hygiene or delayed wound healing
- Existing skin or soft tissue infections in the perineum or lower abdomen
Symptoms and Clinical Presentation
Recognizing the Signs of Pelvic Cellulitis
Patients with pelvic cellulitis typically present with the following symptoms:
- Diffuse pelvic pain
- Erythema and warmth over the affected area
- Swelling and tenderness
- Fever and chills
- Tachycardia
- Malaise and fatigue
- Purulent vaginal or perineal discharge in some gynecologic cases
Advanced or untreated cellulitis may lead to abscess formation, necrotizing fasciitis, or sepsis.
Diagnostic Approaches for Pelvic Cellulitis
Timely diagnosis is vital to prevent complications. A combination of clinical evaluation and diagnostic imaging ensures effective identification and assessment.
Physical Examination
- Inspection of the pelvic area for signs of inflammation or discharge
- Palpation revealing tenderness, warmth, and induration
Laboratory Investigations
- Elevated white blood cell count (WBC)
- Increased C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR)
- Blood cultures for systemic infections
Imaging Modalities
- Ultrasound: To detect fluid accumulation or abscess
- CT Scan: Useful for assessing the depth and spread of infection
- MRI: Superior soft tissue resolution in complex or recurrent infections
Treatment Protocols for Pelvic Cellulitis
Antibiotic Therapy
The cornerstone of pelvic cellulitis treatment is prompt initiation of empiric intravenous antibiotics targeting both aerobic and anaerobic bacteria.
First-line Regimens:
- Clindamycin + Gentamicin
- Ampicillin/Sulbactam
- Piperacillin/Tazobactam for broad coverage
Once culture results are available, therapy should be adjusted based on bacterial sensitivity.
Supportive Care
- Adequate hydration
- Antipyretics for fever
- Pain management with NSAIDs or analgesics
- Monitoring for systemic signs of sepsis
Surgical Intervention
In cases where abscess or necrotizing infection is suspected:
- Surgical drainage
- Debridement of necrotic tissue
- Laparoscopic exploration if pelvic organs are involved
Complications Arising from Untreated Pelvic Cellulitis
- Pelvic abscess
- Necrotizing fasciitis
- Sepsis and septic shock
- Fistula formation
- Chronic pelvic pain
- Infertility if reproductive organs are affected
Prognosis and Recovery Timeline
With timely and appropriate therapy, pelvic cellulitis has a favorable prognosis. Most patients respond to intravenous antibiotics within 48–72 hours. Recovery is typically complete in 7 to 14 days, but close follow-up is required to monitor for complications or recurrence.
Preventive Strategies for Pelvic Cellulitis
Hygiene and Wound Care
- Proper post-surgical wound hygiene
- Regular changing of dressings
- Antiseptic cleaning of any lacerations or abrasions
Medical Risk Management
- Tight glycemic control in diabetic patients
- Early treatment of urinary tract or vaginal infections
- Avoiding unnecessary pelvic instrumentation
Surgical Protocols
- Sterile techniques during surgery and delivery
- Prophylactic antibiotics in high-risk gynecologic surgeries
Special Considerations: Pelvic Cellulitis in Postpartum and Postoperative Patients
Postpartum Cellulitis
Typically occurs within 3–5 days after childbirth, particularly following C-section or episiotomy. Monitoring for fever, foul-smelling discharge, and wound tenderness is essential.
Postoperative Cellulitis
Often results from contamination during pelvic surgeries. Early mobilization, sterile techniques, and perioperative antibiotics significantly reduce risk.
Pelvic cellulitis is a rapidly progressive infection of pelvic soft tissues that demands swift recognition and treatment. Thorough understanding of its causes, risk factors, and management options enables clinicians to mitigate complications and ensure complete recovery. Emphasis must be placed on prevention, especially in surgical and postpartum settings, to curb the incidence and impact of this condition.