Pellagra is a nutritional disorder resulting from a deficiency of niacin (vitamin B3) or its precursor tryptophan. Historically referred to as the “disease of the four Ds”—dermatitis, diarrhea, dementia, and death—pellagra remains a public health concern in regions where diets lack sufficient niacin-rich foods or where chronic illnesses interfere with nutrient absorption.

Understanding the Role of Niacin in the Body
Niacin is a water-soluble B-vitamin essential for the conversion of nutrients into energy. It acts as a coenzyme in redox reactions that are critical for DNA repair, cholesterol metabolism, and cellular function. The human body synthesizes niacin from the amino acid tryptophan; however, this process is inefficient and dependent on adequate protein intake.
Causes and Risk Factors of Pellagra
Primary Pellagra
Primary pellagra occurs due to inadequate dietary intake of niacin or tryptophan. Populations that rely heavily on maize (corn) as a staple food are particularly susceptible, as untreated corn lacks bioavailable niacin.
Secondary Pellagra
Secondary pellagra results from medical conditions or lifestyle factors that interfere with niacin metabolism or absorption:
- Chronic alcoholism
- Malabsorption syndromes (e.g., Crohn’s disease, celiac disease)
- Carcinoid syndrome (increased tryptophan metabolism into serotonin)
- Prolonged use of medications (e.g., isoniazid, 5-fluorouracil, phenobarbital)
- HIV/AIDS
Clinical Manifestations of Pellagra
The disease progresses through recognizable symptoms categorized under the “four Ds”:
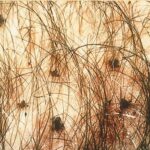
Dermatitis
- Symmetrical, pigmented rash resembling sunburn
- Typically affects sun-exposed areas like the face, neck (Casal’s necklace), hands, and feet
- Scaling, cracking, and thickening of the skin
Diarrhea
- Watery or bloody stool
- Abdominal pain and bloating
- Anorexia and nausea
Dementia
- Confusion, memory loss, irritability
- Depression and hallucinations in advanced stages
- Apathy and psychosis if untreated
Death
- If not promptly treated, the condition may progress to multisystem failure and death
Diagnostic Approaches
Diagnosis is primarily clinical, supported by dietary history and presenting symptoms. However, additional tools may be employed:
- Urinary N-methylnicotinamide test: Low levels indicate deficiency.
- Serum niacin and tryptophan levels (not routinely available).
- Skin biopsy: May show hyperkeratosis and epidermal atrophy.
Differential diagnoses include:
- Pellagroid dermatitis from drug-induced causes
- Photosensitive disorders (e.g., lupus, porphyria)
- Other B-complex vitamin deficiencies
Evidence-Based Treatment of Pellagra
Niacin Supplementation
Immediate administration of nicotinamide (non-flushing form of niacin) is the cornerstone:
- Adults: 300 mg/day in divided doses orally
- Severe cases: May require intravenous administration
Supportive Care
- High-protein diet to boost tryptophan levels
- Vitamin B-complex supplementation
- Treatment of underlying conditions (e.g., alcohol cessation, infection control)
Symptoms generally improve within 24-48 hours of therapy, though neurological deficits may require longer recovery time.
Preventive Strategies
Dietary Interventions
- Diversifying the diet with meat, fish, poultry, legumes, eggs, and fortified cereals
- Nixtamalization of corn (alkaline treatment) to increase niacin bioavailability
Public Health Initiatives
- Food fortification programs in vulnerable regions
- Nutritional education for at-risk populations
- Screening and intervention in alcohol rehabilitation centers and chronic disease clinics
Global Epidemiology of Pellagra
Although rare in developed nations due to widespread food fortification, pellagra remains endemic in parts of Sub-Saharan Africa, Southeast Asia, and rural Latin America. Refugee camps, war zones, and areas suffering from famine are particularly high-risk.
Historical outbreaks, such as in the American South during the early 20th century, underscore the link between poverty, monoculture diets, and pellagra prevalence.
Pellagra in Special Populations
Pregnant and Lactating Women
Niacin requirements are elevated. Deficiency may lead to congenital anomalies or neonatal pellagra.
Elderly Individuals
Age-related absorption decline and polypharmacy increase the risk.
Patients with Psychiatric Disorders
Mental health patients, particularly those with poor dietary habits or institutionalization, face heightened vulnerability.
Pellagra, though largely preventable, continues to pose a threat in nutritionally deprived populations. With early recognition, appropriate supplementation, and public health measures, this potentially fatal condition can be effectively controlled. Awareness, early detection, and dietary interventions are the most effective weapons against this once-forgotten disease.